Image: Shutterstock
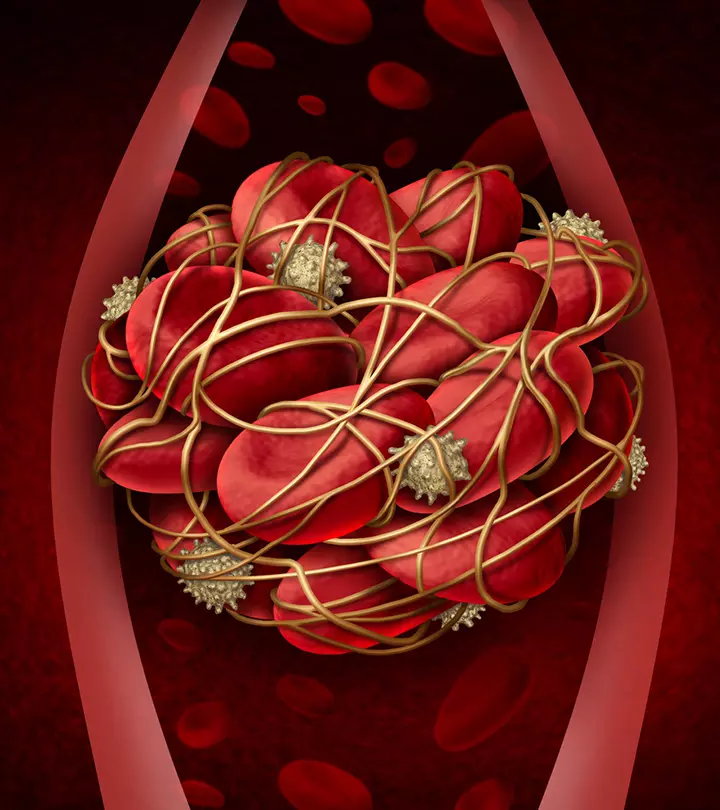
The probability of developing blood clots increases by around five folds during pregnancy. However, although the physiological changes increase the risk of developing blood clots, it is not necessary for all women to develop them. About one or two in 1000 healthy, young pregnant women develop blood clots in pregnancy (1). In addition, certain medical conditions and lifestyle factors may increase the risk for blood clots in pregnancy. Read this post to learn more about the reasons, risk factors, complications, symptoms, treatment, and prevention of blood clots during pregnancy.
What Causes Blood Clots In Pregnancy?
Physiological changes in pregnancy can cause blood clots during pregnancy, childbirth, and three months after delivery due to the following reasons (2):
- Hypercoagulability is the increased tendency to develop blood clots. During pregnancy, the blood may be in the hypercoagulative state as a natural adaptive mechanism to prevent excessive bleeding during delivery and postpartum.
- The growing uterus can press against the blood vessels supplying and draining blood from the legs. Diminished circulation in the lower extremities may cause blood clot formation.
Who Is At A Higher Risk Of Blood Clots?
According to the Royal College of Obstetricians and Gynecologists (RCOG), the following factors and conditions are associated with a higher risk for developing blood clots when pregnant (3):
- History of blood clots or deep vein thrombosis (DVT)
- First degree relative with venous thrombosis
- Older than 35 years
- Three or more previous deliveries
- Wheelchair use
- Thrombophilia
- Heart diseases
- Lung diseases
- Arthritis
- Severe varicose veins above the knee with swelling, redness, or pain
- Overweight (body mass index more than 30)
- Intravenous (IV) drug use or smoking
- Prolonged hospitalization during pregnancy for infections such as kidney infections or appendicitis
- Ovarian hyperstimulation syndrome (OHSS) due to fertility treatment
- Multiple pregnancies
- Dehydration in pregnancy, often due to excessive vomiting in early pregnancy
- Prolonged immobility, such as bed rest or traveling for more than four hours without moving
- Preeclampsia
- Antiphospholipid syndrome (APS)
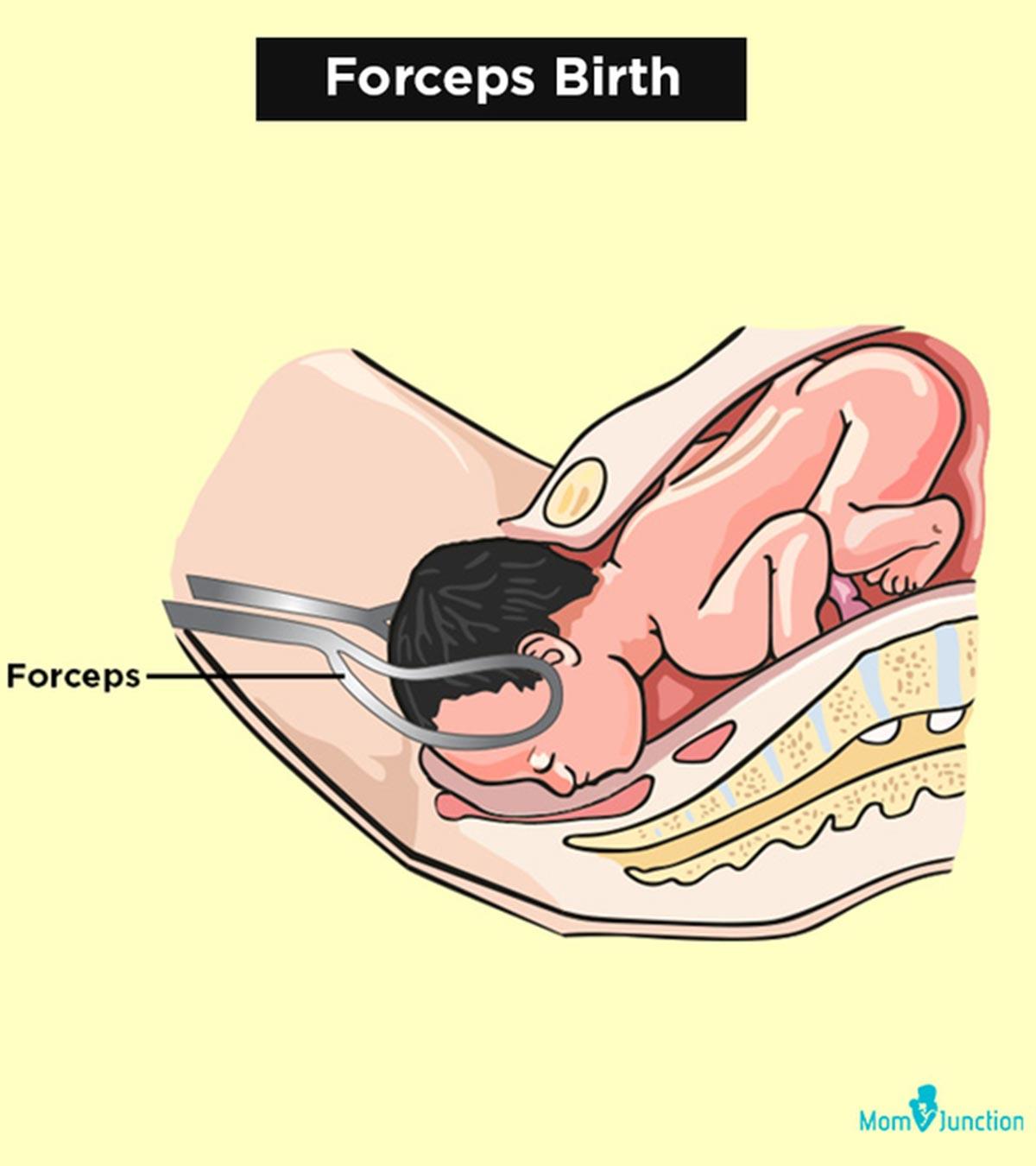
Women who had a long labor (more than 24 hours), C-section, severe blood loss, or received blood transfusion have increased risk for developing blood clots in postpartum. Preventive treatment is often recommended during pregnancy and postpartum for high-risk groups. Hence, inform your healthcare provider if you have any of the conditions mentioned above.
What Are The Types Of Blood Clots?
There are mainly two types of blood clots (4):
- A thrombus is a blood clot that stays where it is formed. The formation of blood clots is called thrombosis.
- An embolus is a blood clot that detaches from where it was formed and moves through the bloodstream. These blood clots can travel to other parts of the body and occlude the blood supply to the respective organs or tissues, causing an embolism.
Around 80% of blood clots in pregnancy are formed in the veins (venous thromboembolism), especially in the legs and pelvic area, while 20% are formed in the arteries (1).
What Are The Complications Of Blood Clots During Pregnancy?
Blood clots in pregnancy can result in the following complications (1) (2) (5):
- Venous thrombosis is the formation of blood clots in the veins. These blood clots can occur in the deep veins of the lower legs, thighs, pelvis, or arms during pregnancy. Pelvic vein thrombosis and ovarian vein thrombosis can cause severe abdominal pain.
- Pulmonary embolism(PE) is caused when blood clots break off and travel through the bloodstream to the lungs, causing a blockage. PE is life-threatening, but the risk for PE is lower if DVT is treated since four in five venous clots are DVT, and one in five is PE.
- Post-thrombotic syndrome(PTS) is a long-term complication of DVT that damages the valves of the leg veins due to clots. This may cause pain and swelling and affect the quality of life.
- Placental thrombosis is the formation of blood clots inside the placenta. This may harm the baby due to inadequate oxygen and nutrient Sometimes, placental blood clots can lead to miscarriage or stillbirth (6).
- Heart attacks are seen in one in six arterial clots due to blockage of the arteries supplying blood to the heart (coronary arteries).
- Stroke is seen in five in six arterial clots that occlude the brain vessels.
Blood clots caused by thrombophilia can cause adverse pregnancy outcomes known as placenta-mediated complications, such as preeclampsia, unexplained fetal loss, placental abruption, and fetal growth restrictions (7).
What Are The Symptoms Of Blood Clots In Pregnancy?
The following signs and symptoms are often observed on the affected limb or area where blood clots are formed in the deep veins (DVT) (8):
- Swelling
- Pain
- Tenderness
- Warmth
- Redness
- Discoloration
The following symptoms are seen if the blood clot moves to the lungs (8):
- Breathing troubles
- Chest pain that increases with cough or a deep breath
- Coughing up blood
- Irregular and fast heartbeat
Seek emergency medical care if you have any of these symptoms. If left untreated, blood clots in pregnancy can be life-threatening for the mother and fetus.
How Are Blood Clots Diagnosed and Treated In Pregnancy?
Compression ultrasound (CUS) is used to rule out suspected symptomatic deep venous thrombosis (DVT). Two-point and three-point CUS is found effective in ruling out DVT. However, the diagnosis method is best decided after examination by a gynecologist.
Blood clots in pregnancy are treated with anticoagulants (blood thinners) such as unfractionated heparin or low molecular weight heparin (LMWH). Heparin is administered through subcutaneous injections (under the skin) on the abdomen. Your doctor will show you how to do these injections and prescribe doses based on individual factors (9).
Heparin does not cross the placenta and is safe during pregnancy. Many mothers may be worried about daily injections on the belly during pregnancy. However, the needles are very short and cannot penetrate below the fatty layer beneath the skin. These medications cannot be given orally since the stomach acids break them down (10).
Anticoagulants, such as warfarin, are available in tablet form but are not safe during pregnancy since they cross the placental barrier. Therefore, warfarin is often prescribed two weeks after delivery when the major risk of bleeding subsides.
How To Prevent Blood Clots During Pregnancy?
Blood clots in pregnancy are preventable. Doctors may recommend prophylaxis (prevention) with anticoagulants for women at a higher risk of developing blood clots.
The following factors can help prevent blood clots in pregnancy (6):
- Inform your doctor about your risk factors and family history of blood clots
- Take anticoagulants as prescribed
- Know the signs and symptoms of blood clots and seek prompt medical care
- Exercise regularly as per recommendations
The American College of Obstetricians and Gynecologists (ACOG) advises pregnant women with high risk for DVT to follow these recommendations while traveling, especially on long trips (11):
- Wear loose-fitting clothes
- Drink plenty of water
- Stretch your legs or walk at regular intervals
- Wear knee-high compression stockings if recommended by your doctor
Do not wear compression stockings if not recommended by your doctor. It can cause more harm than good in some conditions, such as diabetes or blood circulation problems.
Do Blood Clots In Pregnancy Mean A Miscarriage?
Not all women with blood clots have a miscarriage. Blood clots in pregnancy may cause a miscarriage if they block placental circulation. Some rare conditions such as APS can also cause blood clots and recurrent miscarriages (12). However, women with blood clots can be treated and can continue their pregnancy and deliver healthy babies without complications.
Some women may pass lemon-sized blood clots during a miscarriage. These may be products of conception (pregnancy tissue) or clots formed due to bleeding during pregnancy loss. Abdominal cramps or pain and vaginal bleeding may indicate a miscarriage (13).
Frequently Asked Questions
1. What do miscarriage clots look like?
Miscarriage clots may appear dark red with jelly-like consistency along with membrane tissues. However, the appearance may differ depending on the time of its occurrence (14).
2. Are blood clots normal in early pregnancy?
Yes, blood clots may occur during the first three months of pregnancy. Although they are not a complication, it is better to consult an Ob/Gyn to rule out any problems and seek timely help (15).
Although pregnancy increases the risk of blood clot formation, only pregnant women with other risk factors tend to develop blood clots during pregnancy. Hence, discuss your risk factors with your healthcare provider during the initial prenatal visits. Knowing the symptoms can help you seek prompt medical care since blood clots are preventable and treatable.
Key Pointers
- Blood clots in pregnancy can be due to hypercoagulability and diminished blood flow in the lower blood vessels.
- Women with a history of DVT, age more than 35, lung and heart diseases are at a greater risk of developing blood clots in pregnancy.
- Swelling, warmth, and discoloration are signs of blood clots in DVT, while breathing troubles and coughing up blood indicate clots in the lungs.
References
- Does Pregnancy Cause Blood Clots?
https://www.stoptheclot.org/pregnancy/does-pregnancy-cause-blood-clots/ - Venous Thromboembolism (Blood Clots) and Pregnancy.
https://www.cdc.gov/ncbddd/dvt/pregnancy.html - Diagnosis and treatment of venous thrombosis in pregnancy and after birth.
https://www.rcog.org.uk/en/patients/patient-leaflets/treatment-of-venous-thrombosis-in-pregnancy-and-after-birth/ - Blood Clots.
https://familydoctor.org/condition/blood-clots/ - Deep vein thrombosis in pregnancy.
https://www.nhs.uk/pregnancy/related-conditions/complications/deep-vein-thrombosis/ - Blood Clotting & Pregnancy.
https://www.hematology.org/education/patients/blood-clots/pregnancy - The Evolving Story Of Pregnancy Outcome, Thromboembolism And Thrombophilia.
https://www.stoptheclot.org/news/the-evolving-story-of-pregnancy-outcome-thromboembolism-and-thrombophilia/ - Pregnant? Don’t Overlook Blood Clots.
https://www.cdc.gov/ncbddd/dvt/features/blood-clots-pregnant-women.html - How Are Blood Clots Treated During Pregnancy?
https://www.stoptheclot.org/pregnancy/clot_treatment_pregnancy/ - Heparin Use During Pregnancy.
https://www.nbt.nhs.uk/maternity-services/pregnancy/heparin-use-during-pregnancy - Preventing Deep Vein Thrombosis.
https://www.acog.org/womens-health/faqs/preventing-deep-vein-thrombosis - Antiphospholipid Syndrome.
https://rarediseases.org/rare-diseases/antiphospholipid-syndrome/ - Miscarriage.
https://www.betterhealth.vic.gov.au/health/healthyliving/miscarriage - What really happens during a miscarraige.
https://www.pregnancybirthbaby.org.au/what-really-happens-during-a-miscarriage - Blood clots during pregnancy.
https://americanpregnancy.org/healthy-pregnancy/pregnancy-complications/blood-clots-during-pregnancy/
Read full bio of Dr. Uma Mishra