Image: Shutterstock
Pregnancy incontinence or urinary incontinence is the inability to control bowel or bladder function during pregnancy (1) (2). Sometimes women experience urine leakage in small amounts during childbirth (3). In a cross-sectional study conducted with 750 pregnant women, 300 experienced urinary incontinence (4).
Read more about the causes, diagnosis, treatment, and prevention of pregnancy incontinence.
Type Of Incontinence Experienced During And After Pregnancy
The most common urinary incontinence experienced during pregnancy and postpartum is stress urinary incontinence.
Women may leak urine while laughing, coughing, sneezing, or doing physical activity (2).
- During pregnancy, stress urinary incontinence occurs because the growing baby in the uterus compresses the bladder resting under it. This causes extra pressure in the bladder, causing urine leakage more often (2). A cross-sectional study on pregnant women demonstrated that more women experienced urinary incontinence in the third trimester than in the first trimester (5).
- After childbirth, stress urinary incontinence occurs because of stretching and weakening of the pelvic floor muscles (muscles that support the bladder, uterus, and bowels). When the body prepares for birth, and the baby moves down, progesteroneiA female reproductive hormone that plays an important role in menstruation, pregnancy, and breastfeeding levels change, causing the pelvic floor muscles to stretch (6). This means the muscles that control the bladder become weak, leading to incontinence (7).
Causes Of Pregnancy Incontinence
Apart from the growing uterus size during pregnancy and the hormonal effect during childbirth, pregnancy incontinence may also occur for the following reasons (2).
- Pelvic organ prolapse: Childbirth, especially vaginal birth, may weaken the pelvic floor muscles, leading to pelvic organ prolapse. The bladder, uterus, and rectum slip down into the vaginal canal, leading to urinary incontinence (6).
Jennifer, a mother of five shares how she found out about her pelvic prolapse. She says, “This pregnancy was physically painful. I experienced frequent urinary incontinence in the form of constant leakage. I also suffered from constipation resulting in straining and hemorrhoids. But I thought it was normal. My friends were going through the same thing… After a very long pregnancy of over 42 weeks, our lives were blessed with a little baby girl. My urinary incontinence went away, so I thought I had nothing to worry about. But when I got constipated or had a large bowel movement something did not feel right! It was a weird feeling that I had a hard time describing, and it would go away on its own, so I pushed it to the back of my mind… One day, I attended a local woman’s health event that just happened to be about pelvic organ prolapse. It was not a topic that interested me because it did not seem to apply to me. I was young and healthy, after all. Boy oh boy, was I wrong… After I had time to process the information from the program, I realized that I was suffering some prolapse (i).”
- Pelvic nerve damage: Long and difficult vaginal delivery may damage the pelvic nerves, thus affecting bladder function.
- Injury during forceps delivery: In some cases, forceps delivery causes an injury to the pelvic floor and anal sphincter musclesiA group of voluntary muscles around the anal canal that control the release of stool .
Image: Shutterstock
- Prolonged pushing during vaginal delivery may injure the pelvic nerves, causing incontinence.
 Quick fact
Quick factRisk Factors For Incontinence During Pregnancy
Some factors that increase the risk of incontinence during pregnancy are (1) (8):
- Previously weakened pelvic floor muscles
- Constipation because it puts pressure on the pelvic floor
- Urinary tract infection
- Neurological or musculoskeletal conditions, such as arthritis, dementiaiA syndrome characterized by the deterioration in cognitive functions, such as memory and thinking skills , and stroke
- Health conditions, such as diabetes, obesity, and heart disease
- Pregnancy with multiples
- Smoking
Image: Shutterstock
- Sedentary lifestyle
- Having a large baby
- More than one pregnancy (9)
Diagnosis Of Pregnancy Incontinence
Your doctor will take you through a physical examination to check your bladder’s function and exclude other medical conditions. You will also be asked questions related to (10)
- Frequency of emptying your bladder
- Frequency of urine leakage
- Amount of urine leaked
- Other symptoms
The diagnostic tests include (2):
- Urinalysis, where the urine sample is examined for possible infections causing incontinence.
- Ultrasound imaging helps in examining whether the bladder is emptying completely or not.
Image: Shutterstock
- A bladder stress test to check for signs of urine leakage while coughing.
- Cystoscopy involves the insertion of a thin endoscope with a miniature camera in the urethra. It helps examine the inside of the bladder.
- Urodynamics to measure the pressure inside the bladder. During this test, water is filled in the bladder through a thin tube inserted in it.
Treatment And Prevention Of Pregnancy Incontinence
Pregnancy incontinence is usually not treated with medicines. However, some preferable treatment options include the following:
1. Include Kegel exercises: Also called pelvic floor exercises, you can perform them before, during, and after pregnancy to prevent and treat urinary incontinence (2) (7).
Kegel exercises
- Heal the perinealiThe area between the genitals and anus tissue
- Strengthen pelvic floor muscles
- Ensure better urinary control
To perform Kegel exercises (7)
Image: Shutterstock
- Breathe in and out
- Contract the pelvic floor muscles and pull them up and in as if to control the urine flow
- Breathe normally and squeeze and hold for ten seconds
- Then, relax and repeat the process
- Do three sets of ten exercises each, every day
 Quick tip
Quick tip2. Create a bladder diary: A bladder diary is useful in effectively tracking your urinary incontinence. Recording the frequency of urination and tracking the amount, time, and frequency of urine leakage will enable you to understand the severity of the condition and get ready to the bathroom before experiencing the leakage (2).
3. Avoid carbonated or caffeinated drinks because they increase the urge to urinate. Instead, drink water and decaffeinated beverages to enhance your bladder capacity (11).
4. Avoid drinking large amounts of fluid after dinner to reduce urination at night (2).
5. Eat a high-fiber diet to avoid constipation because the additional pressure created by this condition may increase the risk of urinary incontinence (2).
6. Being overweight can increase the pressure on the bladder and worsen incontinence. Therefore, maintaining a healthy weight after delivery may improve bladder control (2).
7. Quit smoking: Smoking increases the risk of chronic cough and irritates the bladder, so quit smoking to improve your urinary incontinence (6).
8. Include regular exercise for at least 30 minutes a day.
9. Avoid exercises involving lifting heavy weights, contact sports, excessive twisting, bouncing, holding breath, curving the back, and standing on one leg for a long time.
10. Do not delay going to the toilet when you are urged to do so.
11. Get treated for urinary tract infection if you have the condition.
Medications and surgery to treat urinary incontinence are required only in some cases. However, it is good to consult a healthcare provider about it (7).
A study was conducted to determine the clinical impact of urinary incontinence (UI) in pregnancy and delivery. UI was most prevalent in the third trimester when compared to the first. Only 13% of women sought medical help to treat UI, as the majority weren’t bothered by UI and believed that the condition would resolve on its own. The below graph depicts the beliefs and help-seeking behavior exhibited by pregnant women. 56% of women who did not seek help believed that the condition would completely resolve or improve in the future.
Beliefs about prognosis of urinary incontinence if help is not sought among non-help-seekers and help-seekers
Source: Back pain prevalence and associated factors in children and adolescents: an epidemiological population study; Revista de Saúde Pública Point to consider
Point to considerSigns To See A Doctor
Image: Shutterstock
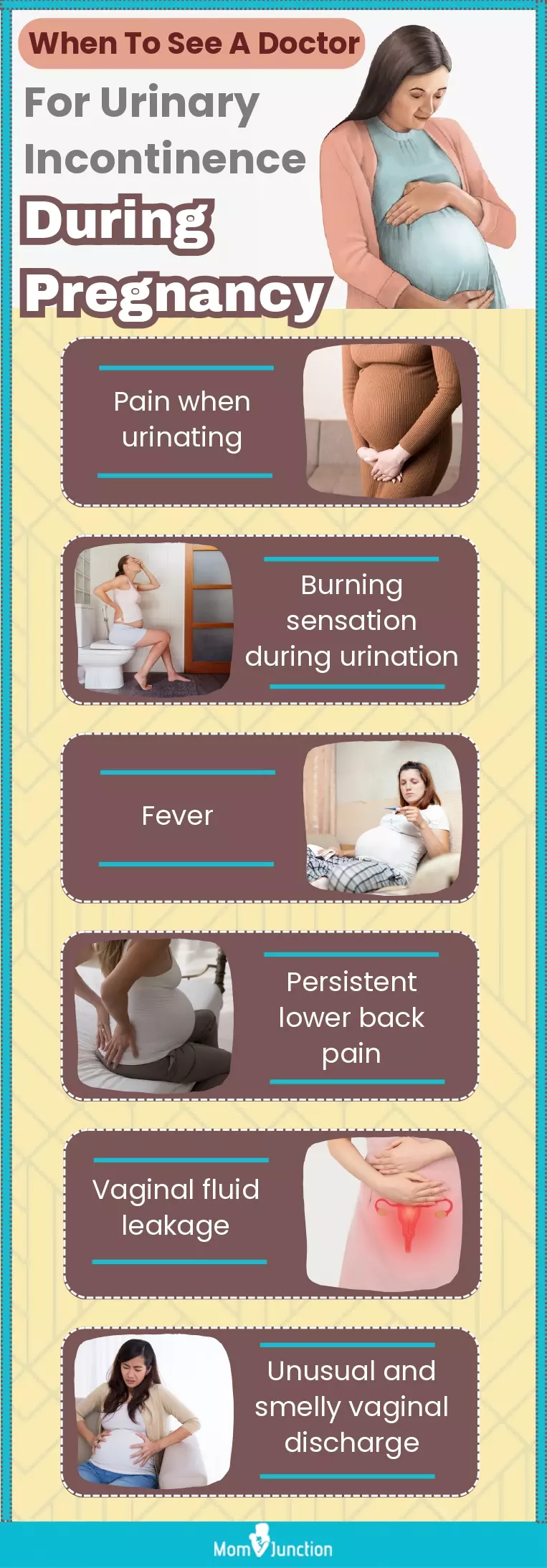
You should consult your doctor if you experience (12)
- Pain or burning sensation during urination
- Fever
- Lower backache that does not get better with rest
- Any fluid leakage from the vagina
- Unusual or smelly vaginal discharge
Frequently Asked Questions
1. Does incontinence go away after the baby is born?
In most women, incontinence goes away in three to six months after childbirth; however, in some women, the stretching and tear of the pelvic muscles do not heal completely. In such cases, it is advisable to consult your healthcare provider. It also helps if you regularly continue practicing Kegel exercises to bring your pelvic floor back to normal (1).
2. How can urinary incontinence be treated after pregnancy?
Straight after birth, give the pelvic floor time to recover. Ice the perineal area for the first few days and have plenty of rest. Then, you can begin with gentle pelvic floor exercises. These exercises may help prevent long-term bladder problems. Simple lifestyle changes may also help urinary incontinence, such as losing pregnancy weight, eating more fiber, drinking more water, and lifting less. However, if it doesn’t get better, talk to your doctor, who may refer you to a specialist. Long-term treatment modalities for urinary incontinence include exercises, medications, or surgery (7).
2. How do I know if I am leaking amniotic fluid or urine?
When the amniotic sac breaks before labor, the amniotic fluid leaks. This leakage or the discharge may seem like a constant trickle or a sudden gush of fluid. This fluid is clear and odorless. However, when urine leaks from the bladder, it is generally little and has a distinct urine smell and yellowish color (13).
3. Is pregnancy incontinence a sign of a more serious problem?
While pregnancy incontinence is bothersome, it isn’t a sign of an adverse health issue. In most cases, pregnancy incontinence symptoms self-resolve after childbirth as the body returns to its pre-pregnancy state. However, consult your healthcare provider if you are experiencing persistent or severe urinary incontinence. In some cases, pregnancy incontinence could be a sign of urinary tract infection or bladder dysfunction.
4. Can pregnancy incontinence affect my ability to give birth?
No clinical evidence suggests that pregnancy incontinence can affect your ability to give a normal birth to your baby. If you have concerns about the impact of pregnancy incontinence on your ability to give birth, discuss them with your healthcare provider.
Pregnancy incontinence might bring a lot of discomfort but is a common condition. It is easy to manage with exercises and lifestyle changes in most cases. However, if your symptoms are concerning, it is good to discuss them with a healthcare provider.
Infographic: Severe Symptoms Of Urinary Incontinence
The growing belly and fetal size often increase the risk of developing frequent urination and incontinence in pregnancy. Simple exercises and changes in lifestyle and eating habits can help manage this condition. But there could be some scenarios when medical treatment may be necessary. The infographic below lists some signs of urinary incontinence that warrant a doctor’s visit.
Illustration: Momjunction Design Team
Key Pointers
- Growing uterus size and hormonal changes during pregnancy can cause incontinence, the inability to control bladder or bowel functions.
- Pelvic organ collapse, nerve damage, prolonged pushing during labor, and injury during a forceps delivery are some factors that may cause it.
- Urinalysis, bladder stress tests, cystoscopy, urodynamics, and ultrasound are some diagnostic methods for pregnancy incontinence.
- Kegel exercises, tracking bladder movements, consuming a high-fiber diet, and avoiding carbonated beverages can help manage incontinence during pregnancy.
- Pregnant women who experience pain or burning sensation during urination, lower back pain, fever, or vaginal discharge should seek medical attention.
Image: Stable Diffusion/MomJunction Design Team
Urinary incontinence during pregnancy may be addressed with the help of kegel exercises. Learn how to perform these exercises correctly while expecting with the help of this video.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My pelvic organ prolapse story of healing and moving forwardhttps://bookishfamily.blogspot.com/2019/02/healing-pelvic-organ-prolapse-rectocele.html
References
- Incontinence during pregnancy.
https://www.pregnancybirthbaby.org.au/incontinence-during-pregnancy - Pregnancy and Bladder Control.
https://my.clevelandclinic.org/health/articles/16094-pregnancy-and-bladder-control - Pregnancy and childbirth.
https://www.continence.org.au/who-it-affects/women/pregnancy-and-childbirth - Ayten Dinç; (2018); Prevalence of Urinary Incontinence During Pregnancy and Associated Risk Factors.
https://pubmed.ncbi.nlm.nih.gov/28675636/ - Eva Martínez Franco et al.; (2014); Urinary incontinence during pregnancy. Is there a difference between first and third trimester?
https://pubmed.ncbi.nlm.nih.gov/25262291/ - Tips to prevent involuntary urine leakage (incontinence) during and after pregnancy.
https://utswmed.org/medblog/leakage-incontinence-during-after-pregnancy/ - Bladder weakness after birth.
https://www.pregnancybirthbaby.org.au/bladder-weakness-after-birth - Aruna Nigam et al.; (2016); Prevalence and risk factors for urinary incontinence in pregnant women during late third trimester.
https://www.ijrcog.org/index.php/ijrcog/article/view/1325 - Childbirth & Incontinence.
https://www.uclahealth.org/medical-services/womens-pelvic-health/childbirth-incontinence - Urinary incontinence.
https://www.womenshealth.gov/a-z-topics/urinary-incontinence#:~:text=As%20many%20as%204%20in%2010%20women%20get%20urinary%20incontinence%20during%20pregnancy.&text=During%20pregnancy%2C%20as%20your%20unbornleaks%20or%20problems%20passing%20urine. - 10 truths: leaking urine in pregnancy and after birth.
https://www.nct.org.uk/life-parent/your-body-after-birth/10-truths-leaking-urine-pregnancy-and-after-birth - Urinary incontinence in pregnancy.
https://www2.hse.ie/conditions/urinary-incontinence-pregnancy/ - Signs of Labor.
https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/signs-of-labor/
Read full bio of Dr. Shashwat Jani
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das