Image: Shutterstock
Hysterectomy is a procedure involving surgical womb or uterine removal. It could also involve the removal of the cervix, fallopian tubesiHollow tubes that connect the ovaries to the uterus and through which the eggs travel to the uterus. , and one or both ovaries, depending on the individual’s medical condition. Pregnancy after hysterectomy is not possible.
Hysterectomy is a major surgery that could be recommended due to various health reasons. Studies suggest that above one-third of women in the US have undergone this surgery by the age of 60 years (1).
Explore more on the key aspects of this hysterectomy and its long-term outlook.
Why Do You Need A Hysterectomy?
Image: Shutterstock
Hysterectomy is a medically necessary procedure to treat health problems affecting the female reproductive system. You might need one if you have any of the following conditions:
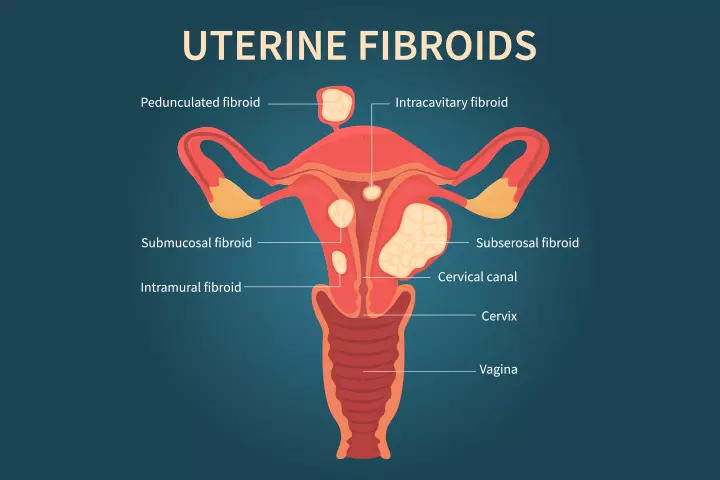
- Heavy or unusual bleeding: Fluctuation in hormonal levels, vaginal infections, fibroidsiBenign tumors that usually grow in the uterus of women of childbearing age. , or cancers can cause excessive and prolonged bleeding (2).
- Uterine fibroids: These non-cancerous tumors report on the uterine wall and may lead to heavy menstrual bleeding and pain (3). According to the US Office on Women’s Health, the prevalence of uterine fibroids is two to three times higher in overweight and obese women.
- Endometriosis: It is a condition wherein the endometrial tissue lining the uterus grows outside of the uterus and on other areas such as the ovaries, fallopian tubes, and outer uterine surface. Symptoms can include spotting or bleeding between menstrual periods, digestive problems, and different kinds of severe pain (4).
- Uterine prolapse: It occurs when the uterus slips down and presses into the vagina. It is likely to happen in women who had prior vaginal births and may also develop due to obesity or aging. It could lead to abnormal vaginal bleeding or discharge and bowel and urinary problems (5).
- Adenomyosis: It is the thickening of the uterine walls wherein the tissue lining grows into the muscular walls of the uterus. It leads to heavy bleeding and severe pain (6).
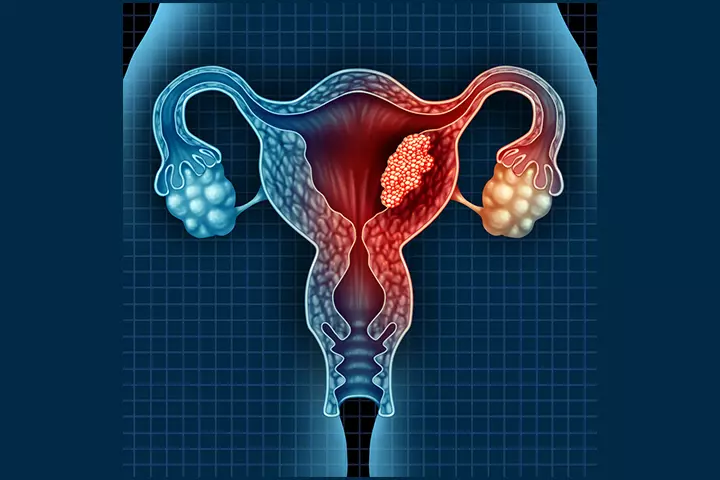
- Cancer of uterus, cervix, ovary, or endometriumiThe inner lining of the uterine wall. : Hysterectomy could be the option if other treatment procedures such as radiation therapy, hormone therapy, and chemotherapy do not work (7).
Image: Shutterstock
- Obstetric hysterectomy. In the case of heavy hemorrhage due to uterus atonyiA condition in which the uterus does not contract properly after childbirth, as a result becomes soft and weak. orplacenta accretaiA condition in which the placenta grows too deeply into the uterine wall and is difficult to detach after childbirth. , hysterectomy is the definitive method of controlling postpartum hemorrhage. This procedure saves undoubtedly mother’s life.
Having a hysterectomy will end your ability to get pregnant. If you plan to become pregnant and cannot go for this procedure, you should consult your doctor for alternatives. For some conditions such as endometriosis, uterine prolapse, and fibroids, there may be less invasive options.
Types Of Hysterectomy
Image: Shutterstock
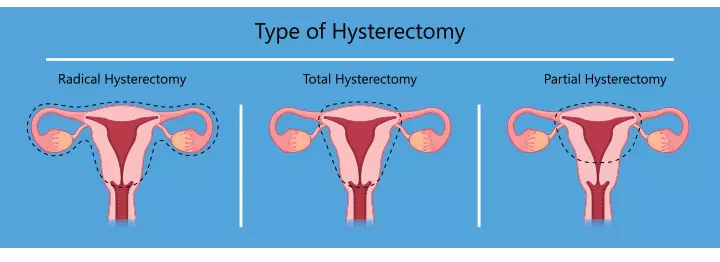
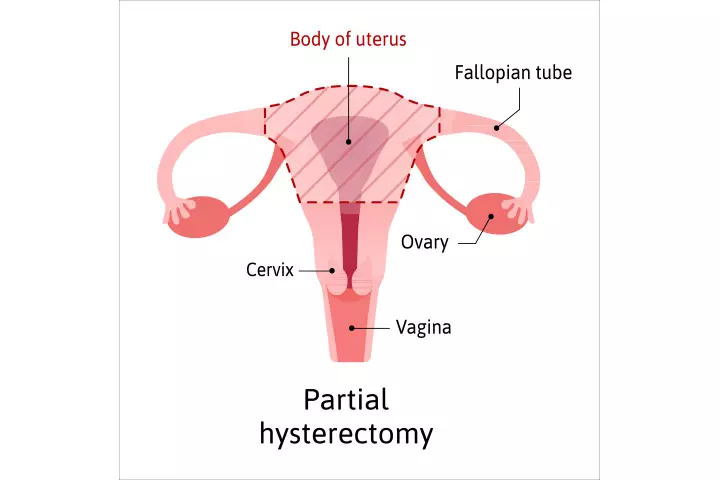
You may require a specific type of hysterectomy depending on why you need it, and how well your reproductive system can sustain it (8).
- Total hysterectomy: It removes the uterus and cervix and is a commonly preferred option.
- Subtotal hysterectomy (also called partial or supracervical): It removes only the upper part of the uterus and leaves the cervix. The ovaries may or may not be removed.
- Total hysterectomy with bilateral salpingo-oophorectomy: It removes the uterus, cervix, fallopian tubes, and ovaries through a prophylactic surgery.
- Radical hysterectomy: It is used to treat cancers. It removes uterus, fallopian tubes, ovaries, the upper part of the vagina, lymph glands, and fatty tissue in the pelvic region.
How Is A Hysterectomy Performed?
A hysterectomy is performed in several ways—through the vagina, abdomen, or by using laparoscopy.
The method depends on your health history and the reason for the surgery (9).
1. Vaginal hysterectomy: A small incision is made near the vagina, and the uterus (or other parts) is removed through it. It is preferred in pelvic relaxation. It takes less time and results in faster recovery. Most women are likely to resume their work or activities sooner than if they had abdominal surgery.
2. Abdominal hysterectomy: It is performed through a regular incision in your lower abdomen, similar to C-section incision. The opening gives a clear view of the pelvic organs. It takes a long time to recover and could lead to complications such as bleeding, wound infection, nerve and tissue damage, and blood clots.
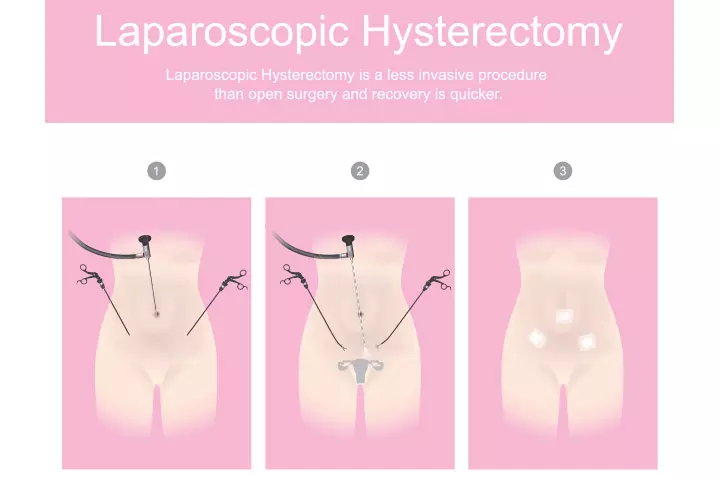
3. Laparoscopic hysterectomy: It is performed by making some tiny incisions in your abdomen. A laparoscopeiAn instrument with a camera used in surgeries that helps doctors to view the pelvic regions without making a large incision. is inserted to view the pelvic organs. Both the procedure and recovery take less time.
Image: IStock
4. Robot-assisted laparoscopic hysterectomy: In this procedure, the surgeon controls a robotic machine to perform the surgery through a small incision in the lower abdomen.
 Point to consider
Point to considerRisks And Complications Of Hysterectomy
As with any surgery, hysterectomy may also lead to some risks and long-term complications (10).
Some of the possible risks with the procedure could be:
- Blood clots
- Bladder or bowel injury
- Infection
- Blood loss that may require transfusion
- Problems while giving anesthesia
Following hysterectomy, you are likely to have some long-term complications too, including:
- Feelings of diminished or lost femininity
- A decrease in sex drive (with the removal of both ovaries)
- Pain during sex (in case of partial vaginal removal)
- Pelvic weakness
- Vaginal dryness (due to low estrogen levels upon removal of ovaries)
- Risk of osteoporosisiA condition in which the bones become brittle and weak, leading to easy fractures. (when ovaries are removed)
 Caution
CautionCan You Get Pregnant After Total Hysterectomy?
You can no longer have menstrual periods and cannot become pregnant after a hysterectomy because the womb (or the uterus) where the baby grows is removed. In this procedure, the whole uterus, including the ovaries and fallopian tubes, are removed (9).
Do You Still Ovulate After A Partial Hysterectomy?
Image: IStock
A partial hysterectomy that leads to ovary preservation and retaining of fallopian tubes could help you ovulate. You may also get pregnant, but the chances that the embryo could survive are rare as it will not have a uterus to implant itself. This may increase the risk of ectopic pregnancy (11) and an emergent situation for a woman’s life.
Ectopic Pregnancy After Hysterectomy
Ectopic pregnancy, also known as tubal pregnancy, develops when a fertilized egg implants and grows outside the main uterine cavity, especially in the fallopian tubes. Ovulation and fertilization occur, but there is no chance for the embryo to develop further. This situation is rare and may be happen when the hysterectomy is performed in luteal phaseiThe second phase of menstruation that begins on day 15 of the cycle and usually ends on day 28 when a woman gets her period. of cycle without a measurement of bHCG in the blood before surgery. It is not possible to carry it to term without a uterus to support its growth. Ectopic pregnancy could be life-threatening and is associated with the following symptoms that may help your doctor diagnose the condition.
- Vaginal bleeding if hysterectomy is partial
- Hemorrhage in the case of rupture of internal tissues
- Severe abdominal pain
- Nausea and vomiting
- Pain in the rectal region, neck, and shoulder
- Extreme fatigue and dizziness
- Shock from the lost blood inside the peritoneal cavityiThe abdominal cavity containing the stomach, intestines, and liver.
Your doctor may usually prescribe methotrexate to remove the fetal tissue. If that does not work, it is surgically removed through laparoscopy or open is it is immerge (12).
Is It Possible To Have A Child After Hysterectomy?
There is a way to have a child through surrogacy wherein someone else carries the baby for you. In this option, your eggs could be harvested for fertility treatment and implanted into a surrogate who can carry the baby.
Another option is to adopt a child if you do not want to consider surrogacy (13).
Frequently Asked Questions
1. Can a uterus grow back after a hysterectomy?
Once the uterus is removed through a hysterectomy, it does not grow back.
2. Where do your eggs go after a hysterectomy?
When the ovaries release eggs, they are likely to float in the pelvic or abdominal cavities where they dissolve and get reabsorbed by the body. It is also possible to harvest them in a lab if you want to consider surrogacy. A fertility specialist can help you in making this decision.
3. Does a hysterectomy shorten your life?
Hysterectomy is likely to enhance the quality of your life as it relieves you from symptoms of serious medical problems. You may enjoy an improved sense of well-being.
Hysterectomy is a major surgery that results in life-changing circumstances. Counseling is necessary before surgery and in follow ups. Patients need to know the cause of hysterotomy and the quality of life after hysterectomy.
4. How long do ovaries work after a hysterectomy?
If your hysterectomy leaves one or both of your ovaries unharmed, then the ovaries can continue to produce the hormone testosterone for up to 20 years (16).
Hysterectomy is a medical procedure performed when a woman has serious pelvic health or other body issues affecting the female reproductive organs. While it could be relieving for some women, some might eventually experience depression due to losing fertility since it is impossible to conceive after a hysterectomy. Moreover, pregnancy after hysterectomy may include ectopic or abdominal pregnancies, leading to life-threatening situations. Therefore, it is vital to speak to your doctor about possible alternatives such as surrogacy or adoption. Nevertheless, ensure routine health check-ups to maintain your healthy self.
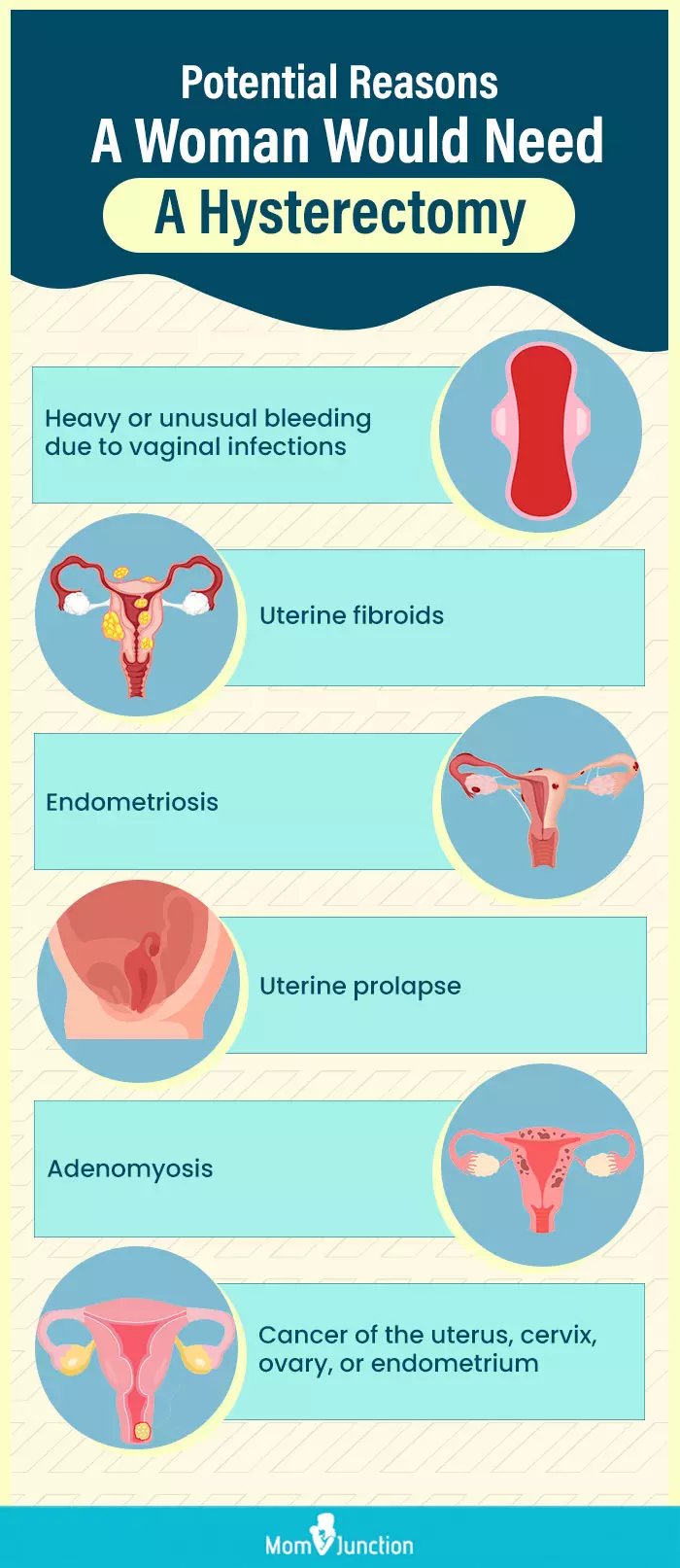
Infographic: Why Would A Woman Require Hysterectomy?
Hysterectomy is an effective surgical procedure involving removing a woman’s uterus. A doctor may advise a total hysterectomy, partial hysterectomy, radical hysterectomy, or total hysterectomy, depending on the severity of the underlying problems requiring uterus removal. Check out the infographic below to learn about the conditions for which the doctor recommends a hysterectomy.
Illustration: Momjunction Design Team
Key Pointers
- Hysterectomy is a surgical procedure that involves removing the uterus or other reproductive organs to treat various health issues.
- A hysterectomy may be necessary for heavy, abnormal bleeding, uterine fibroids, endometriosis, uterine prolapse, or cancer.
- Long-term complications may include decreased sex drive, painful intercourse, pelvic weakness, vaginal dryness, and the risk of osteoporosis.
- Hysterectomy can be performed via the vagina, abdomen, or laparoscopy.
- While it is possible to become pregnant after a hysterectomy, the likelihood of fetal survival is rare.
Can I get pregnant after a hysterectomy? Find out in this informative video! Learn about the risks and potential outcomes of pregnancy after a hysterectomy.
References
1. Margaret A. Olsen, et al.; Developing a Risk Stratification Model for Surgical Site Infection after Abdominal Hysterectomy; Washington University School of Medicine Digital Commons@Becker (2009).
2. Heavy periods; NHS
3. Uterine fibroids; Office on Women’s Health
4. Endometriosis; Office on Women’s Health
5. Uterine prolapse; U.S. Department of Health and Human Services National Institutes of Health
6. Adenomyosis; U.S. Department of Health and Human Services National Institutes of Health
7. Uterine Cancer; U.S. Department of Health and Human Services National Institutes of Health
8. Hysterectomy; New York State – Department of Health
9. Hysterectomy; American College of Obstetricians and Gynecologists
10. Complications – Hysterectomy; NHS
11. Fylstra DL; Ectopic pregnancy after hysterectomy: a review and insight into etiology and prevention; Fertil Steril (2010).
12. Ectopic Pregnancy; University of Rochester Medical Center
13. Preserving Fertility in Women With Cancer; American Cancer Society
14. Recovering from hysterectomy; Dana-Faber cancer institute.
15. Hysterectomy; Cleveland Clinic
16. Hysterectomy; NHS
Read full bio of Dr. Irene (Eirini) Orfanoudaki
Read full bio of Dr. Ritika Shah
Read full bio of Reshmi Das