Image: iStock
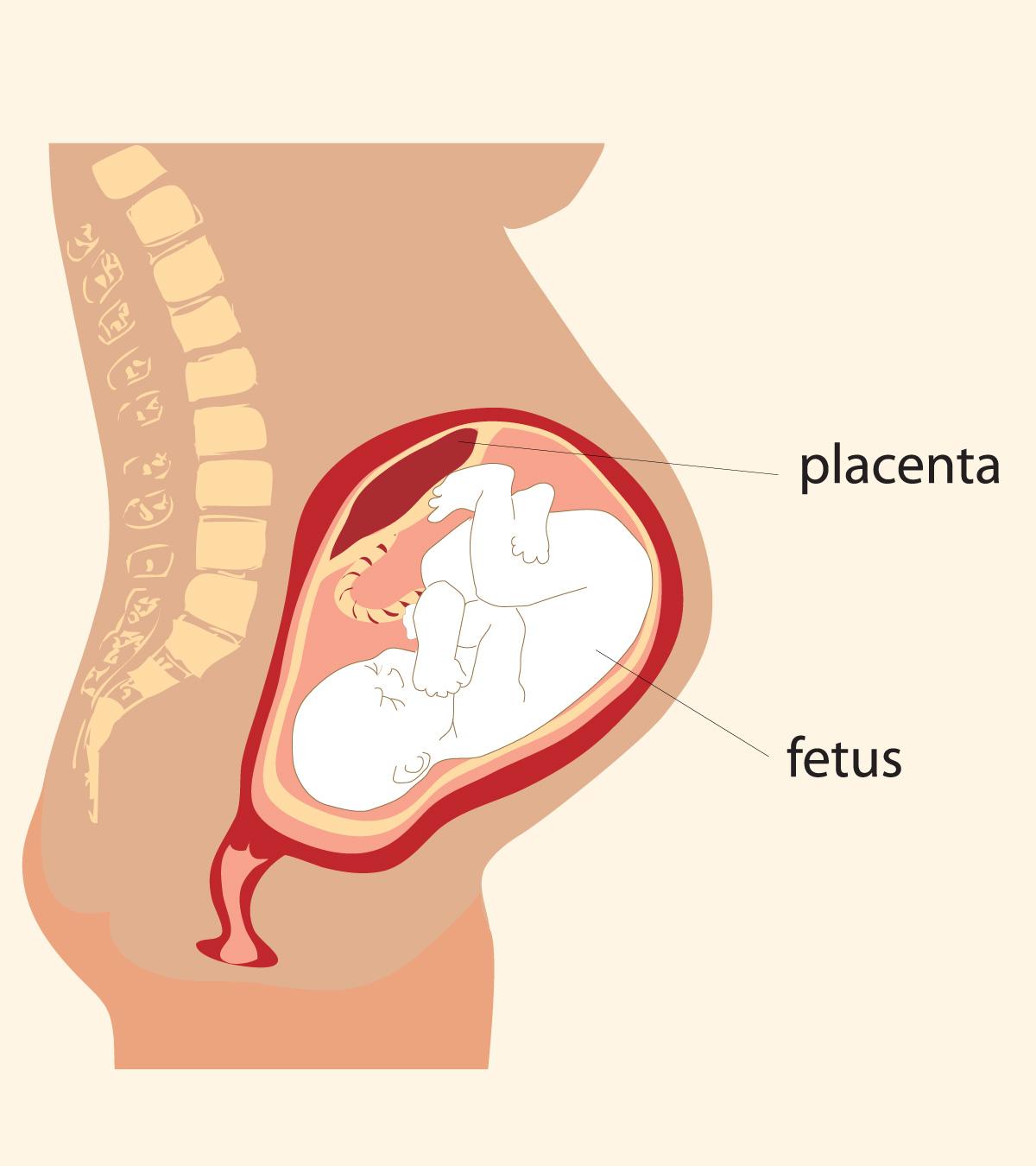
The initial months of pregnancy are crucial to help a fetus develop and decide whether it will be a viable/non-viable pregnancy. The viability of pregnancy depends on several factors, and it is essential for you to understand them. It is also vital for mothers and their partners to understand the importance of prenatal screenings and tests since they can help determine problems early.
Read this post to learn about viable and non-viable pregnancy, how it is determined, reasons that make a pregnancy non-viable, and tips to manage a non-viable pregnancy.
Viable Pregnancy
A viable pregnancy is when the fetus reaches a stage where it is capable of surviving outside the womb, under normal conditions. The viability of a pregnancy is based on many factors, such as the gestational age, birth weight, technological interventions (1) (2).
Ideally, doctors should know if the fetus is viable by 22-25 weeks of gestation, based on ultrasound evaluation.
However, as every pregnancy is different, the viable fetus does not mean that pregnancy will reach nine months and it will result in a full-term baby.
When Is The Viability In Pregnancy Determined?
As every pregnancy is different, the viability of a pregnancy can be determined only after examining the mother and the fetus. Factors on which the viability depends on are (2) (3):
- Mother’s health: Age, reproductive health conditions, previous miscarriages, and the overall health of the woman affects the developing fetus.
- Chromosomal abnormalities: In many cases, the study of chromosomal abnormalities remains unknown. Hence, viability might not be determined sooner.
Image: Shutterstock
- Availability of advanced neonatal care: Depending on the infrastructure and technology used by the hospital, it could either be a timely diagnosis or too late to determine if the pregnancy is viable or not. If a hospital has a tertiary NICU and advanced infrastructure, the viable fetus even at early gestation can be saved in case of preterm labor and delivery.
Image: Shutterstock
These factors could make determining the viability at around 24 weeks difficult, thus delaying the diagnosis. But thanks to the improvements in medical technology, doctors can determine the viability of the pregnancy sooner than later.
When a pregnancy is not viable, it becomes non-viable. Find out more about it next.
Non-Viable Pregnancy
A pregnancy is non-viable when there is hardly any chance of the baby’s survival or when the fetus is not developing.
The result could be an expelled fetus or a living fetus but with limited or no chance of surviving once it is outside the uterus.
In the early weeks, a non-viable pregnancy could lead to an abortion or a miscarriage. Abortions that happen at 21 weeks gestation or later are not common. Data from the CDC’s Abortion Surveillance says that 91% of abortions happen at or before 13 weeks gestation. Only 1.2% of abortions occur at 21 weeks gestation or later.
Abortion trends during early pregnancy.
Source: Abortions Later in Pregnancy; Kaiser Family Foundation/CDCIn the early weeks, a non-viable pregnancy could lead to an abortion or a miscarriage. Bleeding and pain are the typical symptoms of a non-viable pregnancy. Further diagnosis via pelvic ultrasonography and serum hCG measurement are performed to confirm it (4).
A non-viable pregnancy could be due to causes, which we see in the next section.
Causes Of Non-Viable Pregnancy
Various factors could be responsible for a non-viable pregnancy. Some of them are explained below.
- Chemical pregnancy: This kind of pregnancy ends quite early during the first trimester. It happens when the fetus is expelled or dies just after the conception. A chemical pregnancy is also non-viable when the test shows positive results, but there is no gestational saciA structure made of fluid that envelops an embryo in its early stages of development or embryo development (5).
- Molar pregnancy: In this type of pregnancy, the tissue turns into an abnormal growth or tumor in the uterus instead of becoming a fetus. The symptoms include discomfort in the pelvis, vaginal bleeding, vaginal discharge, and signs that indicate hyperthyroidismiA condition where an overactive thyroid gland produces high levels of thyroid hormone (6).
- Ectopic pregnancy: When the implantation occurs outside the uterus, there is no chance of a viable pregnancy. Irrespective of the type of ectopic pregnancy, including cervical, interstitial, or ovarian, the result is non-viable (7).
Jane, a mother of four wonderful children, shares her experience of having an ectopic pregnancy. After a positive pregnancy test, she begins to feel sick around the 7th week. An ultrasound reveals blood in her abdomen. She says, “After reviewing the ultrasound pictures, one of the two doctors from the group came in and explained what was happening. The fetus attached itself to the wall of my left fallopian tube and began to grow there, producing a positive pregnancy test. As it grew, it ruptured my tube, causing blood to leak into my abdomen. He explained that the pregnancy was not viable and that there was no way to move the pregnancy to my uterus. I would need surgery to remove the pregnancy and repair my fallopian tube (i).”
Image: Shutterstock
- Blighted ovum: It is a cause of miscarriage or early pregnancy cause. Other terms for this condition are empty sac and anembryonic pregnancy that occur when gestational sac and placenta are there, but the attached embryo fails to develop (8).
- Congenital anomalies: The WHO states that congenital malformations are among the leading causes of neonatal mortality. However, the laws regarding abortion due to this factor differ across the world. While some don’t allow abortion and encourage the women to carry on with the pregnancy, a few countries keep in mind the psychological condition of the mother and make a decision (9).
- Others: Some other causes of non-viable pregnancy include a premature baby, baby with no heartbeat, abnormal chromosome count, or intrauterine fetal infectionsiWhen the membranes enclosing the unborn child in the womb are infected, adversely affecting the development of the fetus .
In the next section, we talk about the methods to determine the viability of the fetus.
Early Viability Scan
Image: Shutterstock
Early viability scan is done between six and ten weeks. It checks the number of fetuses in the womb, heartbeat, and if everything is normal inside the womb and location of the fetus to rule out ectopic pregnancy. This scan is suggested for pregnant women who are experiencing bleeding or pain and for those who have had a miscarriage previously. The doctor may prefer a transvaginal ultrasoundiA test to examine a woman’s uterus, ovaries, fallopian tubes, and cervix with the help of an ultrasound probe inserted in the vagina to transabdominal, to get better results (10).
The pregnancy is said to be viable if (11):
- The scan detects a gestational sac with a fetal pole and cardiac activity.
- The crown-to-rump length is > 6 mm with a visible heartbeat.
All these can be detected around five to six weeks of pregnancy. If any of the factors mentioned above are not entirely met, it could suggest a non-viable pregnancy. Find out how to determine that in the next section.
Factors Determining Non-Viable Pregnancy
The following factors determine non-viable pregnancy or pregnancy loss. These are checked via a scan (4).
- No heartbeat, and the CRL ≥ 7mm
- No embryo and the mean sac diameter ≥ 25mm
- No embryo and heartbeat after 11 days of the scan, which showed yolk sac and gestational sac
- No embryo and heartbeat after two weeks of the scan, which showed a gestational sac but not a yolk sac
Some findings that could suggest a risky and non-viable pregnancy include:
- No embryo and mean sac diameter between 16mm and 22mm
- No heartbeat and CRL
- Empty amnioniA sonographic finding that shows an amniotic sac but not an embryo
- Six weeks after the period, there is no embryo
- A larger yolk sac, which is greater than 7mm
- Small gestational sac
- No embryo with a heartbeat between seven and 13 days of the scan that earlier showed the gestational sac but not the yolk sac
- No embryo with a heartbeat between seven and ten days of the scan that previously showed a yolk sac and gestational sac
A non-viable pregnancy means there is no chance of the baby being born alive or surviving after it is born. That does not, however, mean that you cannot get pregnant again.
Are There Any Non-Viable Pregnancy Management Options?
Yes. You can follow these non-viable pregnancy management options for a chance to get pregnant even after a non-viable pregnancy or a loss of pregnancy.
- Expectant management: This is a natural method wherein you allow miscarriage naturally, without any medical intervention and use of medicines or surgery. However, if the miscarriage doesn’t happen, then the professional will examine you and decide the next step (12).
- Medicine: A medicine called misoprostol or combined with mifipristone is prescribed for some women to terminate a non-viable pregnancy. Women may experience heavy bleeding or pain in this method. In case the pain becomes severe, consult the obstetrician. It is done under medical supervision (13).
Image: Shutterstock
- Surgery: A simple surgical procedure known as dilation and evacuation or D&E. It is performed to remove the non-viable fetus from the uterus. The procedure is done in just a few minutes (14).
Frequently Asked Questions
1. What is a non-viable birth?
A non-viable birth is a term used to describe spontaneous, unintended fetal morbidity occurring before 20 weeks of gestation as verified by a health care practitioner (15).
2. Can a non-viable pregnancy be misdiagnosed?
Sometimes, a non-viable pregnancy could be misdiagnosed due to misinterpretation of hCG values or an ultrasound scan (16).
3. Can hCG levels rise in a non-viable pregnancy?
No, hCG levels may either decrease or stay unchanged in a non-viable pregnancy except during laboratory errors or an ovarian hyperstimulation syndrome (17).
4. How long does it take for a non-viable pregnancy to be naturally expelled from the body?
The tissues from a miscarriage in a non-viable pregnancy are usually expelled from the body within a few days to a few weeks. However, if it takes longer, medical intervention may be required (18).
5. How soon after a non-viable pregnancy can a woman try to conceive again?
Doctors recommend waiting at least three months to conceive following a pregnancy loss. On the other hand, the World Health Organization advises a six-month waiting period before trying to conceive again (19).
Whether a pregnancy is viable or not depends on factors such as the baby’s gestational age and birth weight. Doctors can determine fetal viability using ultrasound by 22 to 25 weeks of gestation. If pregnancy is non-viable, it could lead to abortion or miscarriage. Blighted ovum, congenital abnormalities, and chemical pregnancy are some reasons that could be responsible for a non-viable pregnancy. Staying informed about viable/non-viable pregnancy essentials can help you make informed decisions when needed.
Infographic: What Are The Best Ways To Handle A Non-Viable Pregnancy?
Although non-viable, a pregnancy loss can be too hard on your mental well-being, especially if you have been trying for a baby for a long time or had recurrent pregnancy losses. Go through the infographic to know the best ways to handle a non-viable pregnancy. Illustration: Momjunction Design Team
Key Pointers
- A viable pregnancy is when a fetus can survive outside the womb under normal conditions, whereas in a non-viable pregnancy, the fetus cannot survive.
- Doctors can check pregnancy viability by 22-25 weeks of gestation through an ultrasound.
- Mother’s health, chromosomal abnormalitiesiA subset of hereditary illnesses resulting from chromosome changes or faulty chromosome organization , and neonatal care are some factors that determine the viability of a pregnancy.
- A non-viable pregnancy can be caused due to reasons, such as chemical pregnancy, molar pregnancy, and so on.
- Non-viable pregnancy could be managed by medicines, surgery, or other management techniques.
Image: Stable Diffusion/MomJunction Design Team
Watch this interesting 3D video and learn how to assess fetal viability! Get an in-depth look at the anatomy and physiology of pregnancy and understand the importance of fetal viability.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Our ectopic pregnancy.http://www.thyhandhathprovided.com/2009/12/our-ectopic-pregnancy-story-1.html
References
1. G. H. Breborowicz; Limits of fetal viability and its enhancement; Early Pregnancy (2001)
2. The Science of “viability”; Later Abortion Initiative (2018)
3. Viability of extremely premature babies; British Pregnancy Advisory Service
4. P. M. Doubilet et al.; Diagnostic Criteria for Nonviable Pregnancy Early in the First Trimester; The New England Journal of Medicine (2013)
5. C. A. Schreiber, M, Sammel, S. L. Hillier, and K. T. Barnhart; A Little Bit Pregnant: Modeling How the Accurate Detection of Pregnancy Can Improve HIV Prevention Trials; American Journal of Epidemiology (2009)
6. Molar Pregnancy; Penn Medicine Lancaster General Health
7. P. L. Edward, S. Bhatt, and V. S. Dogra; Diagnostic Clues of Pregnancy; Radiographics
8. Understanding Blighted Ovum; UC San Deigo Health
9. D. C. Sala and A. R. Abrahao; Obstetric complications in pregnancies with fetal anomalies incompatible with neonatal survival; scielo.br
10. Pelvic Ultrasound: What to Expect; University of Michigan
11. C. Bottomley et al.; The optimal timing of an ultrasound scan to assess the location and viability of an early pregnancy; Human reproduction (2009)
12. Schaefer and D. Lynn; Unrecognised loss: how to best support women experiencing miscarriage; The University of Arizona (2018)
13. K. A. Zikopoulos et al.; Early pregnancy termination with vaginal misoprostol before and after 42 days gestation; Human Reproduction (2002)
14. Dilation and Curettage (D and C); Johns Hopkins Medicine
15. How to Apply for a Florida Certificate of Nonviable Birth; Florida Health.
16. Kurt T. Barnhart; Early Pregnancy Failure: Beware of the Pitfalls of Modern Management; Fertility and Sterility (2013)
17.Müberra Namlı Kalem et al.; ;Problems of modern approaches to management of early pregnancy failure;;(2015)
18. Early Pregnancy Loss;; FAmerican Academy of Family Physicians.
19. Schliep, Karen C et al.; ;Trying to Conceive After an Early Pregnancy Loss: An Assessment on How Long Couples Should Wait;;(2016)
Read full bio of Dr. Ben Abbes Taarji Hicham
Read full bio of Dr. Ritika Shah
Read full bio of Reshmi Das