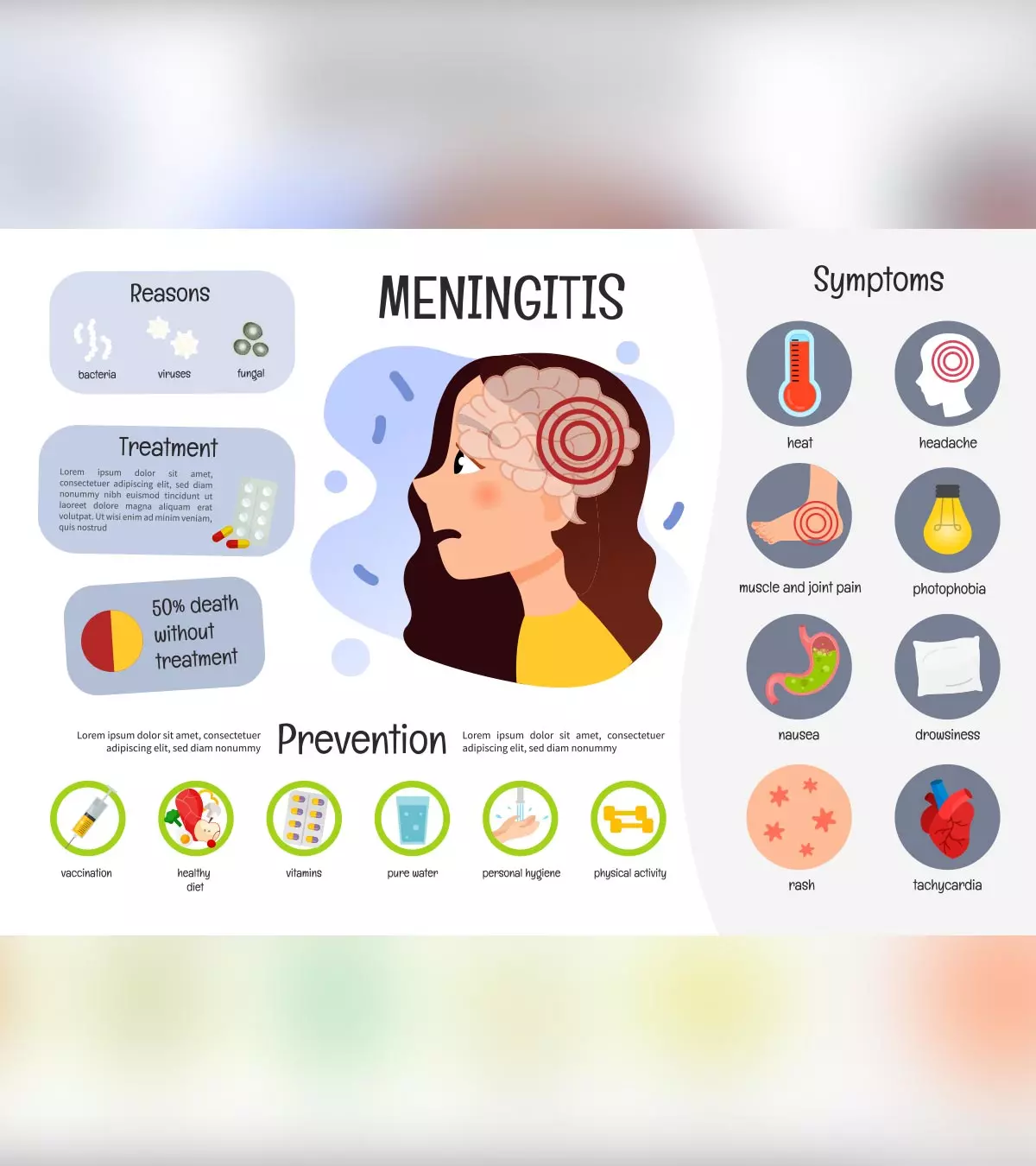
Meningitis is an inflammation of the meninges, a thin membrane surrounding the central nervous system (brain and spinal cord). Meningitis in children may arise due to infections caused by bacteria and viruses and non-infectious aspects, such as tumors and brain injuries. Meningitis might be a life-threatening condition if left untreated, causing long-term complications.
Read on to explore the possible causes, symptoms, treatments, complications, and preventive strategies for meningitis in children.
Causes Of Meningitis In Children
A bacterial or viral infection that propagates through cerebrospinal fluid (CSF) is the most common cause of pediatric meningitis. CSF flows in spaces between the meninges and cushions the brain and the spinal cord. Parasitic and fungal infections may also cause meningitis, and it often affects children with weakened immune systems.
Viruses that cause meningitis include but are not limited to (1):
- Mumps virus (paramyxovirus)
- Poliovirus
- Influenza (flu) virus
- West Nile virusiViruses spread by mosquitoes that rarely cause severe infections such as meningitis and encephalitis.
Bacteria
that cause meningitis include (1):
- Group B streptococcus
- Neisseria meningitidis
- Haemophilus influenzae type b (Hib)
- E. coli
- Streptococcus pneumoniae
- Treponema pallidum (also causes syphilis)
- Mycobacterium tuberculosis (also causes tuberculosis)
Viral meningitis usually needs more supportive care, but bacterial meningitis could be severe and life-threatening if left untreated. The World Health Organization (WHO) reported that bacterial meningitis may cause severe complications in about one in every five cases and result in a fatality for approximately one out of every six affected individuals.
Children can also develop non-infectious meningitis due to the following conditions and factors (2).
- Brain surgery
- Cancers
- Systemic lupus erythematosusiA chronic autoimmune disease causing rashes, swelling, pain, and issues with the internal organ of the body. (SLE)
- Brain injury
Parasitic and fungal meningitis are usually less common. The most common fungal cause is the fungus Cryptococcus found in soil and bird droppings (3). Rat lungworm (Angiostrongylus cantonensis) is a common cause of parasitic meningitis. The parasite transmits through contaminated food and water (4). Exposure to contaminated water bodies, including swimming pools, can expose the child to Naegleria fowleri, a type of ameba that causes amebic meningitis (5).
Risk Factors For Meningitis In Children
Children with weakened immune systems are more likely to develop meningitis than other children.
Pathogens can exist and multiply in other parts of the body, such as the nose and throat, without any symptoms. The following events could cause their transmission (6).
- Sneezing
Image: Shutterstock
- Coughing
- Sharing personal items
- Close contact with an infected person
- Touching contaminated doorknobs, toys, and surfaces and touching eyes, nose, or mouth with unwashed hands.
Untreated cold, sinus infection, or ear infection may cause meningitis as a complication. During these infections, the pathogens could reach the blood and spread to the cerebrospinal fluidiA colorless fluid running through the brain and spinal cord. to cause meningitis later. What may present as a mild cold in an adult, could cause meningitis in infants especially the unvaccinated.
Besides the above mentioned risk factors, meningococcal disease is a possible risk for meningitis in children. The graph below highlights the incidence of the disease in the US across all age groups from 2011 to 2020. As the graph shows, children under 0 to 4 years had an incidence of 0.39%, whereas the incidence among children between five and nine years was 0.07%.
Incidence of meningococcal disease in US across age groups
Source: Meningococcal Disease, Surveillance; CDC/NNDSS Quick fact
Quick factSymptoms And Signs Of Meningitis
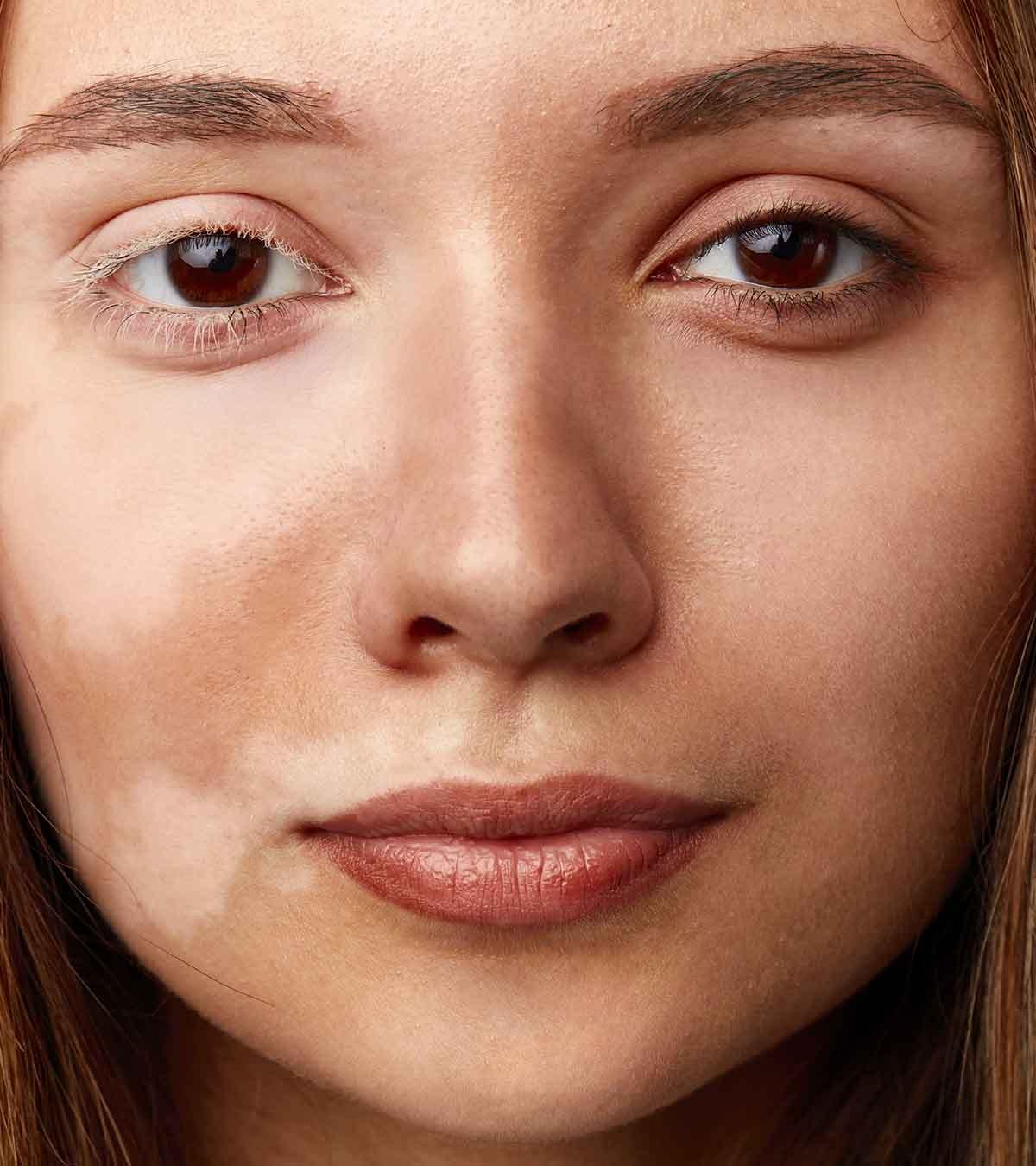
Symptoms and signs may differ in each child, depending on the cause of meningitis. Some may have a rapid onset of symptoms, whereas others may develop symptoms over several days. In most cases, the meningitis symptoms in kids are seen after an episode of a cold and runny nose. Some may have a history of diarrhea or vomiting before the onset of meningitis’ signs and symptoms.
Common signs and symptoms of meningitis could include (7):
- Neck pain
- Stiff neck
- Confusion
- Back pain
- Irritability
- Sleepiness
- Headache
- Seizures
- Fever
- Nausea
- Vomiting
- Photophobia (sensitivity to light)
- Lack of appetite
- Decreased consciousness or drowsiness
- Purple-red skin rashes
These symptoms can also occur in other conditions. Therefore, consult a pediatrician for an exact diagnosis.
Laura Johnson, a mother of five, shares the symptoms her twelve-year-old son manifested after contracting meningitis. She says, “That evening, we awoke to a loud stomping down the hall. I turned the light on, and my son stood at the end, facing the kitchen counter, his back to me, his arms resting at his side. I quickly walked toward him. He wasn’t moving. I turned his body to face me. I noticed he was sweaty, and his eyes were completely black with dilated pupils… He’s burning up hot, we need to cool him down!… My son’s face contorted, he shrieked, but he didn’t resist my moving him. He didn’t stop shrieking until we guided him into a cool shower, hoping it would help him return to us and lower his temperature.”
After repeated instances of seizures, Johnson’s son underwent a spinal tap test for meningitis. She says, “The test returned negative for that type of virus. The official diagnosis was an unidentified viral meningitis that caused, as a side effect, frontal lobe seizures. Recovery from the illness was a few more weeks, but recovery from the seizures? (i).”
When To See A Doctor?
Consult a pediatrician if your child has any of the following conditions.
- Signs and symptoms of meningitis- specifically fever in the first two months of life
- Worsening of symptoms
- The onset of new symptoms
- Not vaccinated
Diagnosis Of Meningitis In Children
Symptoms, physical examination, and medical history could give the doctor clues for determining the presence of meningitis. The following tests confirm the diagnosis (8).
- Blood tests to look for any infections in the blood
Image: Shutterstock
- Lumbar puncture or spinal tap is the only diagnostic test for meningitis. Cerebrospinal fluid is collected from the lower back and evaluated for infectious agents and other indicators.
- CT or MRI scan may be performed to visualize the brain. However, these tests alone cannot confirm meningitis.
- Swabs from the nose, throat, or rectum could be collected to identify the presence of bacteria, virus, or another organism that may have led to meningitis.
Although there are some risks associated with spinal tap procedure, an experienced healthcare provider does the procedure without complications. In some cases, the cerebrospinal fluid analysis results are vital for diagnosing the cause and choosing a specific treatment.
Treatment For Meningitis In Children
Meningitis treatment options may vary depending on the severity, underlying causes, symptoms, and health status of the child.
The following are the common treatment methods for meningitis (9).
- Bacterial meningitis requires immediate treatment with intravenous (IV) antibiotics. Corticosteroid medications could help reduce swelling of the meninges and decrease intracranial pressureiA brain condition characterized by increased pressure in the skull. . These medications could also decrease the risk of complications, such as hearing loss and brain damage. Tuberculous (TB) meningitis may require anti-TB medication for a year, including a combination of antibiotics.
- Viral meningitis may resolve itself without specific treatment in many children. Children with weakened immune systems are treated with antiviral medications. Others may receive symptomatic treatment.
 Quick fact
Quick fact- Fungal meningitis requires IV antifungal medicines.
Image: IStock
Parasitic meningitis usually requires symptomatic treatment with medications prescribed to subdue inflammation and pain.
While your child recovers from meningitis, they also need the following supportive care.
- Bed rest
- Intravenous (IV) fluids or oral fluids to increase fluid intake
- Medicines for fever and headache. Aspirin should not be given without prescription since it may cause Reye’s syndrome in children.
- Ventillator (Respirator (breathing machine) or supplemental oxygen in case of breathing difficulties
- And even close follow up with audiology, ophthalmology, and physical therapies.
You may discuss the risks, possible side effects, and benefits of treatment with the pediatrician since the treatment may vary depending on several individual factors.
Possible Complications Of Meningitis In Children
Untreated meningitis may result in life-threatening complications which might require hospitalization. Children with weak immune systems are more prone to complications of meningitis. Possible long-term complications of meningitis may include (10):
- Seizures
- Hearing loss
- Brain damage
- Various disabilities, depending on the affected area of the brain
Bacterial meningitis is relatively more dangerous and contagious than other forms of meningitis. Always seek medical care if you notice signs and symptoms of meningitis in your child.
Prevention Of Meningitis In Children
Proper handwashing and staying away from an infected person could help prevent the spread of meningitis. Several vaccinations are available to prevent some of the etiologic agents of bacterial meningitis (11).
- Haemophilus influenzae type b vaccine is included in the routine childhood vaccine program, and the first vaccine can be given at two months of age.
Image: Shutterstock
- PCV13 pneumococcal vaccine is given to all children younger than two years, and PPSV23 pneumococcal vaccine is recommended for children with high-risk and older than two years.
- Meningococcal vaccine is given at ages 11 or 12 years and a booster dose at 16 years as a part of the routine vaccine schedule.
- Chickenpox vaccine, MMR vaccine, and annual influenza vaccine (flu shot) can protect against viral meningitis caused by the corresponding virus.
Even if your child is not vaccinated, you can vaccinate them anytime to avoid vaccine-preventable illnesses unless they are currently ill. You may plan your child’s vaccination after discussing it with your child’s pediatrician.
 Did you know?
Did you know?Timely diagnosis and treatment can cure meningitis and prevent its complications. You must ensure that your child completes the recommended course of treatment and follow-up visits to avoid recurrent meningitis. Always vaccinate your child as per the recommendations in your country to avoid vaccine-preventable diseases that can cause meningitis.
Frequently Asked Questions
1. Can a child recover from meningitis?
Yes, a child can recover from meningitis. Timely treatment and care may usually cure bacterial meningitis in seven to 21 days and viral meningitis in seven to ten days (12).
2. What antibiotic treats meningitis?
Antibiotics work for bacterial meningitis. Some of them are Cephalosporin, Vancomycin, Rifampin, Meropenem, and Fluoroquinolones (13). These must only be administered as per a doctor’s prescription.
3. How common is meningitis in children?
Bacterial meningitis affects around 40,000 children under five years annually in the US. Furthermore, 1 per 1000 live births are diagnosed with bacterial meningitis in the first month of life (15).
4. What is the mortality rate for meningitis in children?
Even with timely treatment, the mortality rate for bacterial meningitis in children is 5 to 25% in newborns and 5 to 10% in older infants and children. Consequently, the mortality rate in older infants varies based on the cause. For instance, the mortality rate is 3 to 5% when the infection is caused by Haemophilus influenzae type b and 5 to 10% when the cause is Neisseria meningitidis (16).
5. Is meningitis contagious in children?
Yes, meningitis can be highly contagious. Bacterial and viral meningitis usually spreads through close contact with an infected person, typically through coughing, sneezing, or kissing (17).
Meningitis in children usually occurs in the form of a viral infection or fever. Timely medical intervention and treatment can help cure the sign of this condition and prevent any further complications in your child. Therefore, it is advised to vaccinate your child and consult the doctor if they show any concerning signs or symptoms. In addition, take proper care of your child and teach them the importance of proper hygiene to prevent the chances of meningitis.
Infographic: Caring For A Child With Meningitis At Home
You must aim to provide the best possible home care for a child with meningitis so that the symptoms become manageable and recovery is faster. This infographic provides insights into caring for a child with meningitis at home. Illustration: Momjunction Design Team
Key Pointers
- Children may suffer from meningitis due to viruses or bacteria.
- It can be diagnosed by an MRI scan, blood tests, physical examination, or through symptoms such as neck pain, irritability, backache, sleepiness, and fever.
- Meningitis can be prevented by some vaccine shots and treated with intravenous antibiotics and anti-fungal medications, depending on its type.
Image: Dall·E/MomJunction Design Team
Meningitis is a serious infection of the brain and spinal cord. Learn about its causes, symptoms, diagnosis, and pathology in this informative video and how it can be treated.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My son, possessed;https://laurajohnson-70073.medium.com/my-son-possessed-1d016d97d55e
References
1. Meningitis; Boston Children’s Hospital
2. Meningitis; CDC
3. About Fungal Meningitis; CDC
4. About Parasitic Meningitis; CDC
5. About Amebic Meningitis; CDC
6. Meningitis in Children; University of Rochester
7. Meningitis; Meningitis Research Foundation
8. Meningitis in Children; Johns Hopkins
9. Meningitis; American Academy of Pediatrics
10. Meningitis; NHS
11. Meningitis in Children; Stanford Children’s Health
12. Meningitis in infants and children; Healthy children
13. Liz Smith (2005); Management of Bacterial Meningitis: New Guidelines from the IDSA; AAFP
14. Meningitis; The Royal Children’s Hospital, Melbourne
15. Epidemiology of Meningitis and Ventriculitis in Children; ISPN Guide
16. Meningitis in Children; MSD Manual
17. Meningitis – Causes; NHS
Read full bio of Dr. Tashawna Stokes
Read full bio of Dr. Ritika Shah
Read full bio of Shinta Liz Sunny