Image: iStock
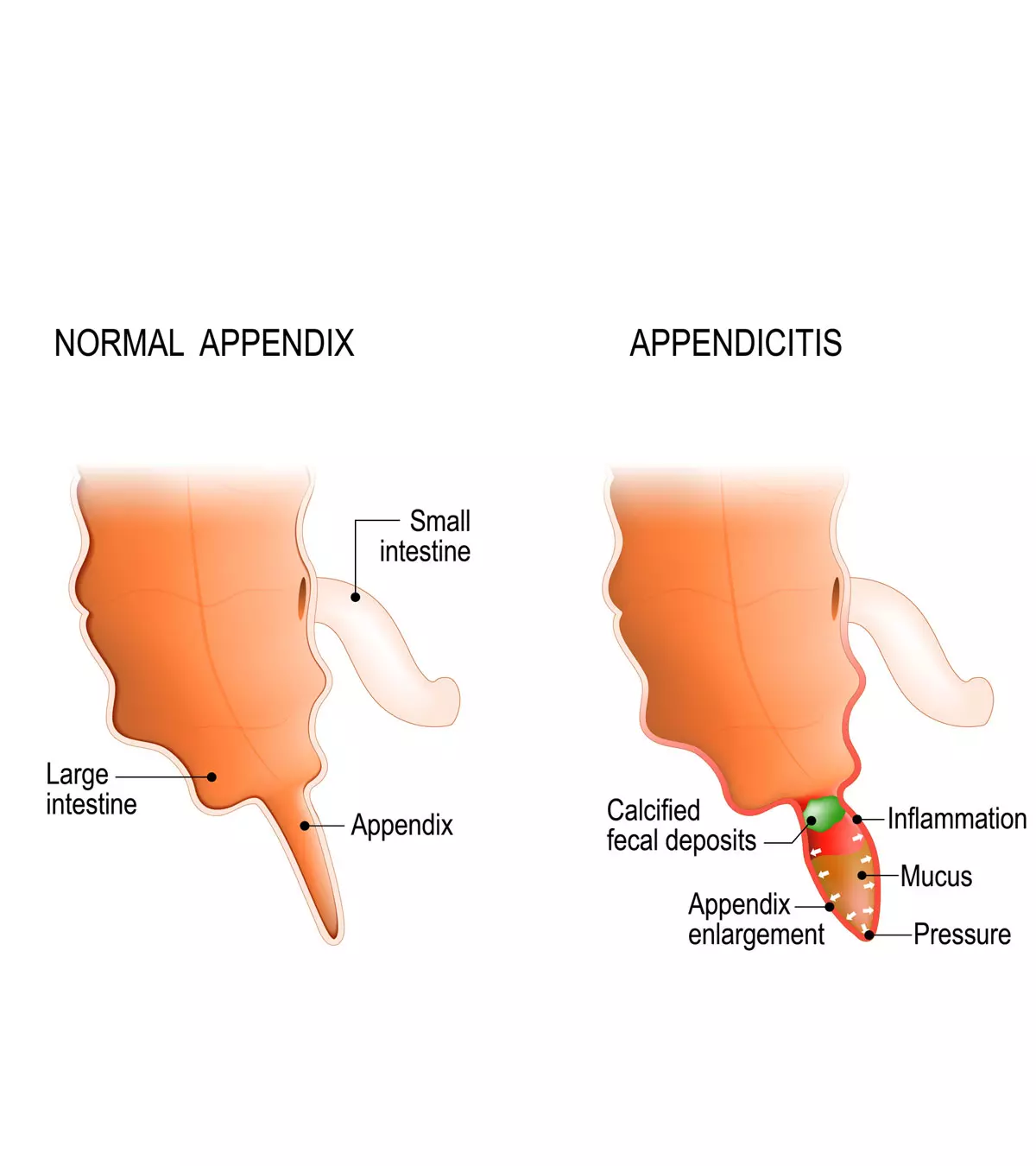
Appendicitis in teens can be presented with abdominal pain that may often begin in the belly button and move toward the right lower quadrant of the abdomen. The appendix is a small, finger-like projection on the intestine at the beginning of the large intestine (colon), and its inflammation is called appendicitis. The research conducted by the Second Hospital of Jilin University reveals that globally, there were 17.70 million new cases of appendicitis reported in 2019, where a noticeably higher incidence rate was observed among individuals aged 15-19. It is the common cause of emergency abdominal surgery in young people aged 11 to 20. Male teens with a positive family history are more likely to develop appendicitis (1).
Removal of the appendix does not impact health since it is a vestigial organ (useless part). However, if left unmanaged, an inflamed appendix can rupture and cause infections and other problems in teens. Read on to know the causes, signs, complications, diagnosis, and treatment for appendicitis in teens.
Signs And Symptoms Of Appendicitis In Teenagers
Image: Shutterstock
The signs and symptoms of appendicitis in teens include (2):
- Abdominal pain due to appendicitis usually begins suddenly in the middle of the tummy, that is, around the naval area, and later causes right lower quadrant pain in the abdomen. The pain usually exacerbates while coughing or walking.
- A low-grade fever follows the abdominal pain and may worsen over time.
- Lack or loss of appetite
- Nausea
- Vomiting
- Diarrhea or constipation
- Abdominal gases (flatulence) and bloating
- Urinary symptoms such as urgency and frequency
- Respiratory symptoms such as shortness of breath
Appendicitis pain can come and go in the beginning when it is felt around the middle of the abdomen
. The pain becomes constant and severe after shifting to the lower right abdomen within hours (2). Chronic appendicitis may show only abdominal tenderness and pain, and other appendicitis symptoms may not be evident. In isolated cases, lower gastrointestinal bleeding, resulting in blood in stool, might be noted. If similar symptoms arise, contact a doctor immediately.
Teenage girls may have appendicitis-like pelvic pain due to some gynecologic disorders. The presence of vaginal bleeding or vaginal discharge may help exclude the possibility of appendicitis.
 Quick fact
Quick factWhen To See A Doctor
Seek immediate medical care if your teen has pain starting from the middle of the tummy and spreading to the right lower part of the abdomen. Avoid giving them food, drinks, or painkillers before consulting a doctor. Early medical attention can be helpful to confirm the diagnosis and begin treatment promptly.
 Be watchful
Be watchfulDiagnosis Of Appendicitis In Teens
Image: IStock
The doctor may examine the child by applying gentle pressure on the abdomen or moving legs to identify the location of the pain. Teenage girls may require a pelvic exam to rule out gynecologic causes of pain on the right side of the abdomen.
The following tests may be ordered to confirm the diagnosis of suspected appendicitis (3).
- Blood tests: It may give evidence of infection such as increased white blood cell count, or C-reactive proteins (CRP)iA proA medical imaging method that generates 3D images of the body's tissues using radio waves, magnetic field, and a computer
tein synthesized by the liver, the levels of which rise due to inflammation. .
- Urinalysis: Urine tests are often performed to exclude kidney stones and urinary tract infections that cause lower abdominal pain.
- Imaging tests: Abdominal ultrasound, computed tomographyiA kind of imaging test used to view detailed images of bones, tissues, organs, and blood vessels. (CT) scan, magnetic resonance imaging (MRI), or an X-ray of the abdomen can be performed to visualize the appendix.
Urological diseases, such as kidney stones and pyelonephritisiA kidney infection. , mimic appendicitis in some cases. Gastrointestinal diseases such as ulcerative colitisiA chronic disease of the large intestine characterized by inflammation and ulcers. and Meckel's diverticulitisiThe congenital gastrointestinal abnormality where there is a bulge present in the lower part of the small intestine. may also show symptoms similar to appendicitis.
Genital diseases such as pelvic inflammatory disease, ovarian torsioniCondition when the ovary and the fallopian tube twist over the ligaments and blood vessels that support them. , ectopic pregnancy in teen girls, and testicular torsioniA condition caused by rotation of the testicle, which hampers blood flow to the scrotum by twisting the spermatic cord. in boys may all present the same problems as seen in appendicitis (4). Your doctor may order a few additional tests to rule out other conditions and confirm the diagnosis of appendicitis.
Appendicitis Treatment In Teens
Surgical removal is the usual treatment for acute or chronic appendicitis. The following are key points about the treatment of appendicitis in teens.
- Surgical removal of the appendix is called an appendectomy, which can be done through laparoscopic (minimally invasive) surgery, also known as laparoscopy or laparotomy (open surgery).
- Laparoscopic appendectomy is less painful and allows for faster recovery. However, it may not be possible in teens with obesity or in cases of peritonitisiInflammation of the tissue that lines the abdomen and abdominal organs. , abscessiA pus-filled pocket, usually resulting from a bacterial infection. , and appendix rupture. Open appendectomy allows washing of the abdominal cavity in cases of rupture (5).
- In a few cases, after imaging tests, if the risk of complications is not seen, then the surgeons may recommend antibiotic treatment and plan appendectomy later. However, treatment decisions and recovery depend on risks and complications.
- Abscesses are often treated with antibiotics with or without draining, and appendectomy is done after controlling the infection.
It is important to seek medical care on time. Early intervention may help in faster recovery –within two to three days of hospitalization. Rupture of the appendix may require more days of hospitalization and could increase the risk of surgical complications (1).
Lifestyle Changes For Teens After Appendectomy
The following lifestyle modifications and home remedies can be useful in post-appendectomy days (6).
- Take medications on time: You should give pain relievers and other medications as per prescription. If your teen still has pain or other symptoms, then call the doctor .
- Plan the diet: Your teen may require small portions of frequent meals initially. Also, encourage them to drink plenty of water to avoid constipation. Drinking alcohol should be avoided since it may interfere with medications. Avoid caffeinated drinks as they may cause constipation.
- Avoid strenuous activities: Always seek the doctor’s advice to return to regular physical activities after surgery. The teen should also avoid strenuous activities, such as lifting groceries, moving furniture, lifting children, etc., for around six weeks. Walking is one of the exercises allowed before six weeks of surgery. The teen may walk and climb stairs in moderation as per the doctor’s advice.
Image: IStock
- Do not drive: It is advised not to drive until the first postoperative visit.
- Support abdomen while coughing: Placing a pillow on the abdomen and applying a little pressure could help reduce pain while coughing or laughing.
- Take rest: You may encourage your teen to take rest and sleep well after surgery to enhance the healing of wounds.
Image: Shutterstock
Call the doctor immediately if your teen has a fever, increased pain, redness, and abdominal swelling at the site of surgery.
Once the surgical wound and the intestines have healed, the teen can return to their normal eating and exercise routine.
 Point to consider
Point to considerCauses Of Appendicitis In Teenagers
Inflammation of the appendix can be caused by its obstruction. Obstruction or blockage of the appendix can be caused by (7):
- Lymphadenitis (inflammation of the lymph nodes)
- Intestinal worms
- Foreign bodies
- Bezoars (collection of indigestible materials in the digestive tract)
- Hardened fecal matter
- Trauma to abdomen
Obstruction may lead to infection due to bacterial growth and result in the accumulation of pus inside the appendix
. If left untreated, it can lead to the rupture of the appendix.
Types Of Appendicitis In Teens
Teens can have any of the following types of appendicitis (8).
- Acute appendicitis: This is an acute inflammation of the appendix with sudden onset of symptoms. It is more common and requires immediate treatment.
- Chronic appendicitis: Chronic inflammation of the appendix may show mild symptoms and often comes and goes. The pain can be severe or dull, and these episodes can be recurrent.
Risks And Complications Of Appendicitis In Teens
Untreated appendicitis may result in complications including (9):
- Rupture: Inflamed appendix may result in rupture or perforation around 36 to 72 hours after the onset of symptoms. A few children may have a small rupture, while some may have spillage of a large amount of pus and feces into the abdominal cavity (10). It can be fatal and will require emergency surgery for the removal of the appendix and cleaning of the abdominal cavity.
- Peritonitis: This may happen after the rupture of the appendix. In this condition, the peritoneum (lining of the abdominal wall) gets infected from the infected contents of the appendix. Peritonitis can be associated with severe pain, rebound tenderness, shortness of breath, rapid heartbeat, and high fever.
- Appendicular abscess: This is the collection of pus in the abdomen and the most common complication of acute appendicitis. The pus requires surgical draining with tubes and treatment with antibiotics.
How To Prevent Appendicitis?
Image: IStock
There is no proven way to prevent appendicitis (11).
Some studies show that a high fiber diet may reduce the risk for appendicitis. It is noted that the occurrence of the condition is low in countries where people consume fiber-rich foods, such as fruits and vegetables. However, more studies are needed to prove the effectiveness of high fiber foods in the prevention of appendicitis (12).
Some home remedies, such as consuming garlic, ginger tea, mint, etc., are followed by people, but they have not been scientifically proven to cure appendicitis. Giving oil massages or applying heat on the abdomen is not recommended by experts.
Frequently Asked Questions
1. How do I check for appendicitis at home?
It is not possible for one to check for appendicitis at home. The doctor will help you diagnose appendicitis through physical examination, blood tests, urine tests, or other advanced imaging tests.
2. What foods make appendicitis worse?
Researchers have established that appendicitis may be more common in people who consume a low-fiber diet (13).
3. What are the stages of acute appendicitis?
Appendicitis is medically described in three stages based on its clinical severity and microscopic appearance. The first stage is a normal appendix, followed by uncomplicated acute appendicitis and complicated appendicitis (14). Rarely acute appendicitis can lead to intestinal obstruction. Contact your doctor immediately for a timely diagnosis and treatment.
4. How long can I have appendicitis without knowing?
The symptoms of acute appendicitis aggravate quickly, while those of chronic appendicitis come and go and, therefore, may often be undiagnosed. Nevertheless, one cannot ignore the suddenly escalating symptoms and require immediate medical attention (15).
Your teen may have appendicitis if they experience abdominal pain in the middle of the stomach, which may be accompanied by low-grade fever, nausea, vomiting, poor appetite, and other symptoms. In such cases, do not give your teen pain medications or antibiotics without first consulting a doctor. The removal of the appendix is the most common treatment and can entirely treat appendicitis in teens. However, if left untreated, it can lead to complications. Therefore, if your teen complains of severe abdominal pain, contact a doctor promptly.
Infographic: Tips On Lifestyle Modification For Teens Post Appendectomy
The doctor may suggest a surgical procedure when appendicitis becomes chronic and begins to impact your child’s routine. This infographic brings simple home care measures after appendectomy surgery; guide your teen to follow these to facilitate quick recovery and avoid post-surgery complications. Illustration: Momjunction Design Team
Key Pointers
- Appendix is a protrusion of tissues near the colon, which when inflamed can cause appendicitis.
- Abdominal pain, loss of appetite, nausea, vomiting, and low-grade fever are some symptoms of appendicitis in teens.
- Early medical diagnosis with scans or lab tests and treatment can help prevent complications such as rupture, abscess, or infection of the abdominal wall.
- Usually, the treatment involves antibiotic administration followed by surgical removal of the appendix (appendectomy).
- A healthy, well-balanced diet, appropriate rest, and walking help with a speedy recovery after appendectomy.
Image: Stable Diffusion/MomJunction Design Team
This informative video explains about appendicitis, its causes, signs and symptoms, diagnosis, and treatment. Get the facts to help you understand and manage this condition.
References
- Appendicitis; Stanford Medicine Children’s Health
- Symptoms; Appendicitis; The National Health Service
- Matthew J. Snyder, et al.; Acute Appendicitis: Efficient Diagnosis and Management; The American Academy of Family Physicians
- Joel P. Thompson, et al.; Mimickers of Acute Appendicitis; Journal of The American Osteopathic College of Radiology
- Treatment for Appendicitis; The National Institute of Diabetes and Digestive and Kidney Diseases
- Caring for myself after Laparoscopic Appendectomy; Michigan Medicine; University of Michigan
- Symptoms & Causes of Appendicitis; The National Institute of Diabetes and Digestive and Kidney Diseases
- A. L. van den Boom, et al.; Interobserver variability in the classification of appendicitis during laparoscopy; British Journal of Surgery
- Complications; Appendicitis; The National Health Service
- Appendicitis revisited: New insights into an age-old problem; Contemporary Pediatrics
Appendicitis; Johns Hopkins Medicine - Rizkiasa Nurafitha, et al.; Relationship of eating habits to acute appendicitis in children: a literature review; Journal of International Surgery and Clinical Medicine
- Boyke Damanik, et al.; Relation between Fiber Diet and Appendicitis Incidence in Children at H. Adam Malik Central Hospital
- Medan North Sumatra-Indonesia; Bali Medical Journal
- Acute appendicitis; Global Alliance for Infections in Surgery
- Signs of appendicitis you shouldn’t ignore; Wexner Medical Centre, OSU
- Kids Health Information: Appendicitis; The Royal Children’s Hospital Melbourne
- Appendicitis in Kids and Teens (for Parents); Nemours KidsHealth
- Appendicitis; Boston Children’s Hospital
Read full bio of Dr. Richard Mario Lurshay
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak