Image: Shutterstock
Breastmilk is important because it offers infants complete nutrition for their growth and development. However, if breastfeeding is not possible on demand, mothers should learn how to store breastmilk.
Storing breastmilk allows mothers the flexibility to feed their babies in their absence or when they cannot nurse. For example, if you are a working mother who has to leave your baby with a caregiver or are unwell and timely breastfeeding becomes difficult, you could feed the stored milk to your baby.
However, to ensure that the milk is expressed, collected, and stored properly and retains all its nutrition, you need to take the necessary precautions. This post provides you with complete information on the safe collection and storage of breastmilk.
Expressing Breastmilk
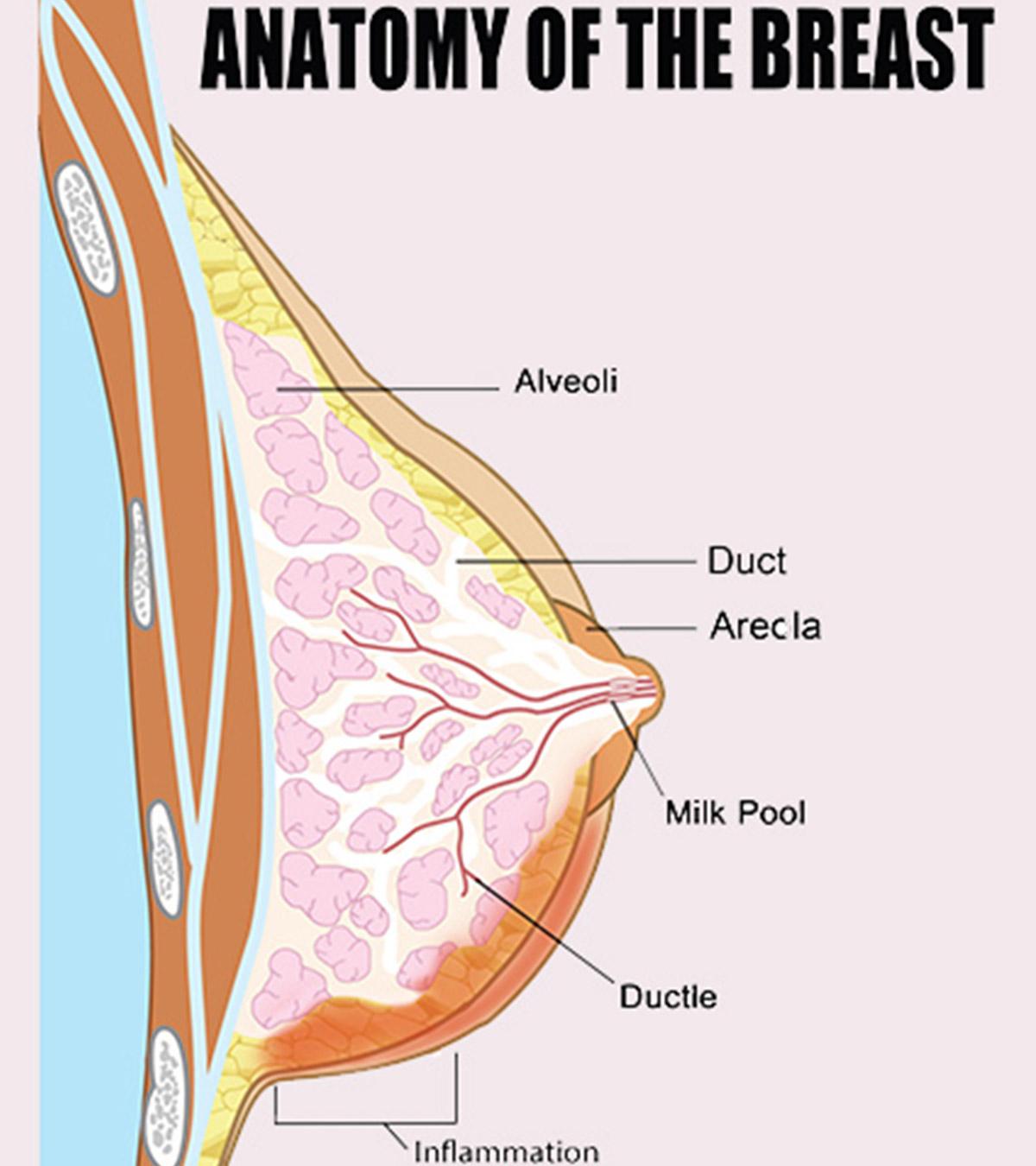
Expressing breastmilk is a way of squeezing milk from your breast so that you can store it for your baby to feed later. You can hand-express or use a manual pump or an electrical pump (1).
You may express milk for any of the following reasons (2):
- If your baby is not able to suck properly
- If she is a premature baby
- If you or your baby are hospitalized and you cannot feed all the time
- If you are a working mother and may have to leave your baby in a creche
- If studies or other commitments bind you
- If you feel your breasts are uncomfortable and too full
- Some mothers may store breast milk for emergencies
- If you may want to use your breast milk to mix with your baby’s solid foods (3)
Different types of pumps suit different women. Therefore, you consult your doctor or try a pump on before you take one. Below are the different ways of expressing breastmilk (4) (5):
| Type | How Does It Work | What Does It Involve |
|---|---|---|
| Hand expression | Massage and compress your breast using your hand to squeeze milk. | Thumb above the nipple at the edges of the areola, or about 2 cm from the nipple, and the forefinger below. Push back against the ribcage, then together toward each other, then forward |
| Manual pump | Use your hand and wrist to manage the hand-held device for pumping the milk | You should have enough practice, coordination, and skill Useful for occasional pumping when you are away from your baby Can cause a higher risk of breast infection. |
| Electrical pump | Works on battery or plugs into an electrical outlet. | Pumps one breast at a time or both breasts at the same time. Easier to handle for mothers Double pumping can express more milk in less time, helpful if you a full-time employee. Equipment should be cleaned after every use. |
Collecting Breastmilk
Collecting breastmilk is an art. Though it takes time to learn this art, you will be able to accomplish it soon by simple steps given below:
- Rinse your hands properly using soap and water
- Wash the breast pump parts and collecting bottles using the dishwasher and hot water. Clean using a towel and air dry them. If your baby is ill or premature, you should sterilize the breast pump parts.
- Carefully read the instructions on the pump parts and accordingly clean them every day (6).
- Practice pumping breastmilk first thing in the morning, when there is highest supply (7). Use one breast to feed your little one and the other to pump the milk. You can also pump the breastmilk for a short while when your baby skips the feed. Use a proper breast shield that fits in comfortably with your nipple.
- Working mothers can teach their babies to bottle feed. You should wait for 2 to 3 weeks before you introduce your baby to the bottle (8). If you have any other problems with breastfeeding, check with the doctor or the lactation consultant.
- Pump milk every three hours when you remain away from your baby. Pump for 10 minutes during breaks and 15 minutes during lunch using a good pump. Doing likewise will help to protect your breastmilk supply. You can breastfeed your baby in the evening after work or on holidays to maintain a proper milk supply and bond with your little one (9).
Which Kind Of Containers Can Be Used To Store Expressed Breastmilk?
You may have worked hard to collect breastmilk. Now, you have to ensure to store it properly. If you are confused about what kind of containers to use, you should read below (1) (10):
Bottles:
- Hard-sided plastic or glass containers that have well fitting lids. However, glass bottles are better than plastic ones.
- Wash the containers with soap and hot water. Wash them well and allow them to air dry before use.
- You can also use dishwasher and water to rinse the containers.
- You should not fill the container up to the brim, instead, leave an inch space on the top as milk expands when it freezes. Store in 1, 2 and 3oz increments.
Note: Plastic bottles and their components turn brittle on freezing and can break easily. Glass bottles may also break if not handled properly. For instance, when they have too much milk, you drop them or knock them over. Don’t store breastmilk in broken bottles.
Bags:
- You will get specially designed milk freezer bags to store breastmilk.
- Fill about 2 to 4 ounces (60 to 120 ml) of milk in the bag to offer it in a single feeding.
- Squeeze out any air that is on the top and leave about one inch as milk expands after freezing.
- Keep the bags at the back of the freezer since the temperature remains consistently cold.
Do not use plastic bags or disposable bottle liners. They possess a high risk of contamination, and moreover, they tend to leak and are less durable. Some plastics will also destroy nutrients in the milk.
How To Store Breast Milk?
Store your breastmilk in a tidy glass or hard-sided plastic BPA-free bottle. You can also store in milk bags that are specially made for freezing breastmilk (10) (11) (12).
After Pumping The Milk:
- Mention the date on the milk storage container. Write your baby’s name if you keep your child in a creche.
- Slightly spin the bottle to blend the creamy part of the milk with the rest of the milk. Avoid shaking the bottle. It can decompose some valuable components of the milk.
- Place the milk in the refrigerator soon after it is expressed. If you do not have a freezer, you can use an insulated cooler temporarily.
- Take containers according to your baby’s feed and fill them individually, like one for one feed. You may begin with 2 -4 ounces (59-118 milliliters) and then slowly adjust as required. Do not store more than 1 to 2 ounces (30-59 milliliters) in a feed.
Freezing Milk:
- Tighten the bottle caps or bag lids until the milk is frozen completely.
- Leave an inch or more at the top of the container as milk expands after freezing.
- Place the milk at the back of the freezer as it is cooler compared to the rest.
- You can freeze the milk for six months or deep freeze for a year.
Thawing And Heating Milk:
- Label the milk containers with the date it was expressed. Always use the older milk first.
- Breastmilk does not require warming. Few mothers prefer serving it chilled, and some prefer to serve it at room temperature.
- Thaw the milk container by pouring warm running water on it and then place it in a bowl of warm water.
- Do not keep the container in a microwave as it can destroy the milk and can also burn your little one.
- Spin the milk and test its temperature by taking a drop on your wrist. It should be warm but not hot.
- You can use thawed milk before 24 hours, and you should not freeze it again.
Guide For Storing Breastmilk:
Here is a simple guide that helps you understand how you can store breastmilk carefully.
| Where | Temperature | Time | Comments |
|---|---|---|---|
| At room temperature (fresh milk) | 66° to 78° F (19° to 26° C) | 4 hours (ideal) up to 6 hours (acceptable)* | Contents should be covered and kept as cool as possible; covering the container with a damp towel may keep milk cooler. |
| Insulated cooler bag | 5° -39° F (-15° -4° C) | 24 hours | Keep ice packs in constant contact with milk containers; limit opening cooler bag. |
| In a refrigerator | 72 hours (ideal) up to 8 days (acceptable)** | Collect in a very clean way to minimize spoilage. Store milk in the back of the main body of the refrigerator. | |
| Freezer (compartment of refrigerator) | 5° F (-15° C) | 2 weeks | Store milk away from sides and toward the back of the freezer where temperature is most constant. Milk stored longer than these ranges |
| Freezer (compartment of refrigerator with separate doors) | 0° F (-18° C) | 3 – 6 months | is usually safe, but some of the fats break down over time. |
| Deep Freezer | -4° F (-20° C) | 6 – 12 months |
* The preference is to refrigerate or chill milk right after it is expressed.** Eight days acceptable if collected in a very clean, careful way.Table Source
Guide For Storing Thawed Breastmilk
| Room temperature (60°F – 85°F) (16 – 30°C) | Refrigerator (39°F or colder) (up to 4°C) | Any freezers | |
|---|---|---|---|
| Thawed breastmilk | 1 to 2 hours is an ideal storage time. Up to 3 to 4 hours is acceptable. | 24 hours is ideal to refrigerate | Avoid refreezing. |
The above guidelines differ with your premature baby. It is better for you to check with your healthcare provider for the storage guidelines.
Tips To Encourage Your Let-Down Reflex While Expressing Breastmilk
You may feel pain when your breasts eject milk, and the pain is transient. The milk ejection reflex or the letdown reflex is set by the oxytocin hormone which stimulates the muscle cells in the breast to eject the milk.
Certain techniques may help to encourage the letdown reflex while expressing breastmilk. For instance (13):
- Try expressing the milk in a warm, quiet and relaxed area which is all away from distractions. Breathe deeply and slowly. You can also prefer having a warm glass of drink before expressing and listen to a gentle music. Take a warm shower or use warm face washers before expressing the milk helps as warmth always helps.
- Gently massage your breasts by giving strokes toward the nipples and roll the nipples between fingers. If you cannot squeeze out the milk by massage, you can trigger the let down by a touch on your breasts.
- Think about your baby and her feed; it will help you to express the milk.
- Having a support also helps. Some mothers feel that they can manage better when they have a partner or friend who encourages them.
Milk Supply And Your Baby’s Needs
- A healthy milk supply remains the same for six months of complete breastfeeding.
- In the initial weeks, babies eat often and also grow quickly.
- Around 3 to 4 months, the baby’s growth rate slows down. If she gains weight rapidly hereafter, it may lead to obesity. The milk supply which is established in the initial days continues to satisfy your baby until six months (14).
- On average, women make about 19 – 30 oz milk every day (15). Infants between 1 to 6 months drink about 19 to 30 oz milk every day. The average size of every feed is 3 to 5 oz (16).
Breastmilk Taste And Odor Changes
Causes Of Milk Taste And Odor Changes (17) (18): Changes in your breastmilk taste and odor can be due to mother’s diet, medications, and milk exposure to cold temperature.
Odor Due To Lipase – Few mothers produce milk that gives an off-odor on freezing. It is because of the lipase enzyme present in the breastmilk. The odor smells rancid or unpleasant on thawing. Though it is safe to drink, some babies may refuse because of the odd taste.
Odor And Taste Test Before Freezing – Collect 1 to 2 bags of breastmilk and freeze for at least five days. You should then evaluate the taste and odor and check whether your baby can drink.
Eliminate Lipase-Induced Milk – If you observe a change in taste and odor of the milk on freezing, you should scald it before you freeze. Scalding the milk after it freezes will not help.
Scalding Fresh Milk – Heat milk in a pot until you see small bubbles at the edges. Now, remove the milk and keep it for freezing. Scalding will take away some useful components fro the breastmilk, so you should prefer giving fresh breastmilk.
Special Cases
Mothers whose babies are in NICU (neonatal intensive care unit) require to express and store more milk. In regular freezers, lipolysis may take place when milk is stored for a long time. But, NICU freezers can store milk at intensive cold temperatures and will not affect the milk. The milk odor and taste will not change at these temperatures that will be around -70° to -80° C (19).
In such a case, you should consult NICU lactation consultant to develop a plan for storing breastmilk.
Frequently Asked Questions
1. How Much Breastmilk Can You Store In The Freezer?
Few women will pump large volumes of breast milk to freeze. You can store up to 2 to 4 ounces (60 to 120 milliliters), as any more will be wasted. You can also pour the breast milk into an ice cube tray which is rinsed thoroughly with hot water. Freeze them and once they turn hard, keep in freezer bags. In this way, you can also keep a count of cubes that are required to make one feed.
2. Is It Normal For The Frozen Breastmilk To Change Color?
Frozen breastmilk may be slightly different from the fresh milk; however, it does not mean it is bad. It is quite normal for the fresh milk to look orangish, and mature milk looks slightly bluish, yellowish or brownish on refrigeration. It will also separate into the creamy top layer and a lighter-colored layer. You should then swirl it lightly so that the milk mixes properly.
Thawed milk tastes soapy and smells different because the fats breakdown in the milk. It is safe for babies to consume the milk after thawing. If your baby doesn’t drink this milk, you can scald the milk and then quickly cool and freeze it. Doing this will switch off the enzyme, which usually breaks down the fats in the milk.
3. Is It Safe To Microwave The Breastmilk?
If you microwave the milk, it will develop hot spots in the bottles. It can be very dangerous when you feed the baby. Instead, you should hold the bottle under warm running water, swirl the container and then give it to your baby.
Instead, you can also use bottle warmers.
4. Is It Safe to Offer Cold Expressed Breastmilk For Your Baby Soon After Refrigeration?
It will not make any difference and also there is no evidence that babies require warm milk. However, most babies prefer milk which is at body temperature. The safest way is to warm the milk by placing it is a bowl of warm water and then offer it to your baby.
5. How Much Breastmilk Is Sufficient For A Single Feed?
It cannot be estimated as babies feeding habits differ from each other. Young ones can just take a small volume, a few milliliters in a single feed whereas older ones can take more. Also, your little one’s appetite may by more on some days and less on other days. Therefore, a rough rule of thumb is to take at least 100 milliliters, plus little extra for each feed. You can later estimate from your baby’s feeding habits.
6. How Can You Feed Expressed Milk For Your Baby?
The common way to offer expressed breastmilk is through a bottle. The alternatives are a special feeding cup, a plastic syringe, or an egg cup. These feeding methods through may be new, are the best for preterm or ill babies who have not learned to feed effectively.
7. Can You Defrost Frozen Breastmilk?
Once the milk is frozen, you can only defrost it before you serve it your baby. Use it straight away after defrosting. Frozen milk is also better than formula milk. Do not freeze milk once it is thawed. You can store the thawed or frozen milk in refrigerator, but cannot refreeze them.
8. Can You Cup Feed With Expressed Breastmilk?
Cup feeding can only be done under a proper supervision of a nurse. Do not give your baby in a cup until you feel confident about it. It can endanger your baby as it may cause choking.
9. Can You Mix Freshly Expressed Breastmilk With Stored Milk?
You can mix freshly expressed milk with frozen milk that is expressed on the same day. But, you have to refrigerate the fresh milk separately and then add to the earlier stored frozen milk. You should not add warm milk to frozen milk as it thaws the frozen milk.
If you cannot breastfeed your baby on demand, storing the breastmilk is a good option. It allows you to offer your baby breastmilk even in your absence. Ensure that your hands and bottle are thoroughly clean before collecting the milk. The collected breastmilk can then be stored at room temperature for four hours or in the freezer for two weeks. If you plan to offer your baby expressed breastmilk, ensure your baby knows to bottle-feed. Always follow proper guidelines for breastmilk storage and speak to a lactation consultant for any queries.
References
- Proper Storage and Preparation of Breast Milk.
https://www.cdc.gov/breastfeeding/recommendations/handling_breastmilk.htm - Expressing and storing breast milk.
https://www.nhs.uk/conditions/baby/breastfeeding-and-bottle-feeding/breastfeeding/expressing-breast-milk/ - Working Together: Breastfeeding and Solid Foods.
https://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Working-Together-Breastfeeding-and-Solid-Foods.aspx - Breastfeeding – expressing breastmilk.
https://www.betterhealth.vic.gov.au/health/healthyliving/breastfeeding-expressing-breastmilk - Pumping and storing breastmilk.
https://www.womenshealth.gov/breastfeeding/pumping-and-storing-breastmilk - How to Keep Your Breast Pump Kit Clean: The Essentials.
https://www.cdc.gov/healthywater/hygiene/healthychildcare/infantfeeding/breastpump.html - Pumping and Hand Expression Basics.
https://wicbreastfeeding.fns.usda.gov/pumping-and-hand-expression-basics - Breastfeeding and going back to work.
https://www.womenshealth.gov/breastfeeding/breastfeeding-home-work-and-public/breastfeeding-and-going-back-work - Pumping Strategies for the Working Mother.
https://lactationmatters.org/2012/05/17/pumping-strategies-for-the-working-mother/ - Breast milk storing.
https://health.clevelandclinic.org/how-to-store-your-breast-milk-safely-infographic - Storing Human Milk.
https://llli.org/breastfeeding-info/storing-human-milk/ - Breastmilk: Pumping, Collecting, Storing.
https://www.stanfordchildrens.org/en/topic/default?id=breastmilk-pumping-collecting-storing-90-P02385 - Health: Breastfeeding – Milk Expression and Storage.
https://scdhec.gov/health/family-planning/breastfeeding/health-breastfeeding-1 - How Much and How Often to Breastfeed.
https://www.cdc.gov/nutrition/infantandtoddlernutrition/breastfeeding/how-much-and-how-often.html - Milk Production and Your High-Risk Baby.
https://www.stanfordchildrens.org/en/topic/default?id=delayed-or-not-enough-milk-production-90-P02390 - Infancy.
https://pressbooks.oer.hawaii.edu/humannutrition2/chapter/13-infancy/ - 3 Things That Can Impact Breast Milk Taste & Smell.
https://www.medela.com/en-us/breastfeeding-pumping/articles/pumping-tips/3-things-that-can-impact-breast-milk-taste-and-smell - Milk Issues.
https://llli.org/breastfeeding-info/smell-human-milk/ - Caroline Steele; (2018); Best Practices for Handling and Administration of Expressed Human Milk and Donor Human Milk for Hospitalized Preterm Infants.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6129589/
Read full bio of Melissa Kotlen