Image: Shutterstock
Strokes in teenagers are an uncommon health condition that has serious consequences. It is one of the top ten causes of death among adolescents (1). So what is this condition?
A stroke occurs when the blood supply to the brain is interrupted. The brain requires a constant supply of oxygen to function; this oxygen is delivered by blood. Therefore, when any factor alters the blood flow, there could be a decrease in oxygen supply to the brain, leading to the death of the brain cells.
Brain stroke is a serious condition that requires prompt medical attention. Delayed diagnosis and management could have fatal results. Read on to know more about brain strokes in adolescents, their causes, risks, symptoms, diagnosis, treatment, complications, and prevention.
Causes And Risk Factors For Stroke In Teenagers
Image: IStock
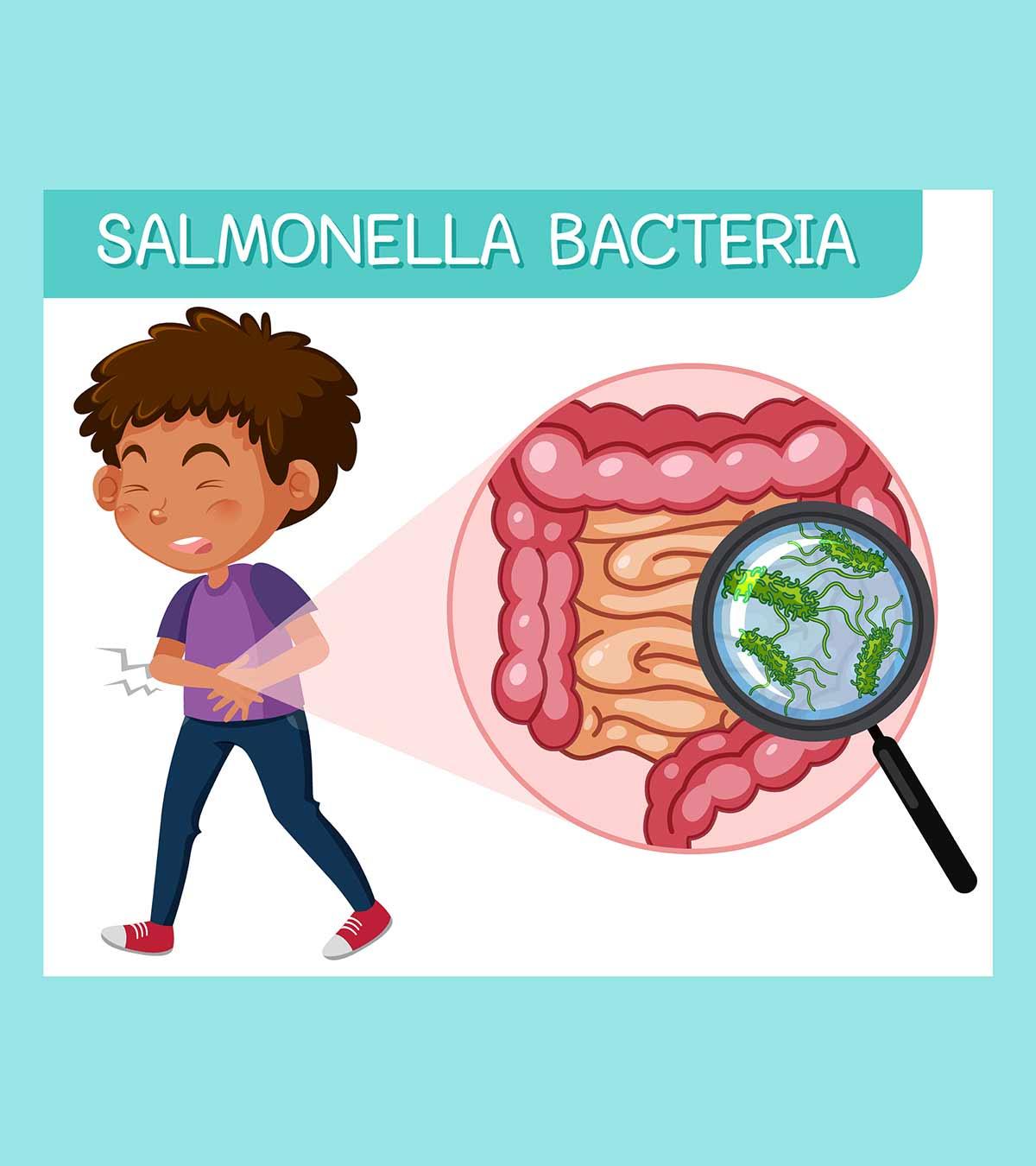
Any blockage or delay in the blood supply of the brain may result in a stroke. If the brain’s blood supply is interrupted by a blocked blood vessel, it is called ischemic stroke, and if it occurs due to a bleeding in the brain, it is called a hemorrhagic stroke.
If the blood supply to the brain is temporarily blocked, teens may experience a mini-stroke (transient ischemic attack or TIA). In such cases, teens may have stroke-like symptoms that usually resolve within the next 24 hours. If the symptoms and disabilities are minimal, it is called a minor stroke. A minor stroke may still require further evaluation to prevent recurrent strokes. According to the US Centers for Disease Control and Prevention (CDC), one out of four strokes are recurrent.
Here are some conditions that may increase the risk of stroke in teens (2).
- Heart diseases
- Head injuries and other injuries
- Blood disorders such as sickle cell diseaseiAn inherited set of blood disorders that cause the red blood cells to be hard, sticky, and sickle-shaped in appearance. and thalassemiaiA hereditary condition in which the body does not produce enough hemoglobin and is characterized by fatigue, paleness, and slow growth.
- Dehydration
- Metabolic disordersiA group of disorders that interfere in the metabolism of the body, thus leading to diseases such as diabetes or cardiovascular diseases.
- Infections such as encephalitisiAn inflammation of the brain caused by infection or autoimmune disease. and meningitisiAn inflammation of the membranes of the brain and spinal cord due to an infection.
- Congenital disabilities (birth defects)
- Hypertension (high blood pressure)
- Genetic disorders like Moyamoya, a condition that affects the arteries in the brain
- Blood clotting issues
- Blood vessel anomalies, such as vasculitisiA condition causing inflammation of the blood vessels, which leads to the thickening of their walls and narrowing of the passage. and dissectioniA tear in the inside wall of the artery, causing blood to enter between the layers of the artery and separating them.
Some teens may develop strokes without any known risk factors and causes. However, teens with known risk factors should take necessary precautions to prevent stroke.
 Be watchful
Be watchfulTypes Of Stroke In Teenagers
Three different types of strokes may affect infants, children, and teenagers (3):
- Arterial Ischemic Stroke (AIS): It occurs when a blood clot obstructs arteries in the brain. It is notably prevalent among younger patients.
- Cerebral Sinovenous Thrombosis (CSVT): It is an ischemic stroke variant where blood clots in the brain prevent the drainage of blood from the veins into larger areas known as venous sinuses.
- Hemorrhagic Stroke (HS): It occurs when blood leaks into brain tissue (intracerebral hemorrhage), the fluid-filled brain-surrounding spaces (subarachnoid hemorrhage), or the ventricles (intraventricular hemorrhage).
Signs And Symptoms Of Stroke In Teenagers
Image: IStock
The signs and symptoms of stroke may vary depending on the underlying cause, severity, and the part of the brain involved. Teens may have stroke symptoms similar to adults. These may include (4):
- Altered mental state
- Confusion
- Sleepiness
- Seizures
- Severe headache
- Tendency to use only one side of the body or the inability to use one side of the body
- Vision problems, such as blurred vision and eye movement problems
- Vomiting
- Swallowing difficulties
- Mood or behavior changes
- Numbness or weakness on the face, a part of the body, or one side of the body
- Dizziness
- Loss of balance and coordination often resulting in walking difficulties
- Issues with speech and language
- Loss of consciousness
Stroke symptoms and signs can be easily remembered by the acronym FAST, and you may call emergency medical care if your child has these symptoms.
- F for face drooping. A common sign of stroke is drooping or numbness of one side of the face, resulting in uneven smiles.
- A for arm weakness. Weakness or numbness of one arm is seen in most cases. A teen may not be able to lift the arm, and the affected arm drifts down while they try to lift it or the inability to actively move one side of the body.
- S for speech difficulties. Slurred speech could be due to stroke in otherwise normally speaking teens. They may even fail to repeat simple sentences in severe strokes.
- T for time to call emergency care (911). You may note the time of the symptoms and contact emergency medical care even if the symptoms mentioned above go away.
The acronym can be particularly useful if your teen has known risk factors, such as heart problems. Early medical care and intervention could improve the outcome.
Complications Of Stroke In Teens
Image: IStock
Severe strokes that last for a longer time may cause permanent brain damage. Mini-strokes usually may not cause any permanent disabilities. The following complications due to brain damage may occur in some teens (5).
- Cognitive impairmentiA disorder in which a person starts to lose memory, has trouble remembering or learning things, and cannot make decisions.
- Paralysis or weakness of a part or side of the body
- Severe vision problems
- Language and communication issues
- Memory-related issues, such as memory loss
- Psychological problems
The severity and type of complication may vary based on multiple factors, including the type of stroke, part of the brain affected, and the time taken to commence emergency treatment.
Diagnosis Of Stroke
Image: IStock
Analysis of symptoms and health history can be the initial step in diagnosing stroke in teens. Doctors may ask a few questions to identify or exclude the possible causes. A set of physical examinations, including neurological examination and visual examination, is done to determine the part of the brain affected.
The following tests are ordered to confirm the diagnosis of stroke (1).
- Brain imaging, such as computed tomography (CT) scan and magnetic resonance imaging (MRI) scans, help visualize the brain.
- Magnetic resonance angiography (MRA) and digital subtraction angiography (DSA) are diagnostic imaging techniques to assess abnormalities of the brain’s blood vessels.
- Magnetic resonance venography (MRV), an MRI test conducted for specific veins.
- Blood tests are done to look for infection and inflammation markers, clotting problems, metabolic conditions, and genetic conditions, such as sickle cell disease.
- Lumbar puncture (spinal tap) is often performed to evaluate the cerebrospinal fluidiA clear fluid that surrounds the brain and spinal cord and provides them protection from injury. (CSF) and look for brain infections.
- Electroencephalography (EEG) is often ordered to analyze the brain’s electrical activity, especially if your teen has seizures.
- Echocardiography to visualize cardiac structure and function and electrocardiography (ECG) to look for heart rhythm are done to check for heart problems, which are a common cause of stroke.
- Pulse oximetry is performed to ensure that there is enough oxygen in the blood.
These are necessary examinations to identify the underlying cause and location of the stroke. However, healthcare providers may order additional tests, depending on various factors, such as the symptoms and results of other tests.
 Things to know
Things to knowTreatment For Stroke In Teens
You may call emergency medical care if your teen has signs of stroke since early interventions are most effective. The following treatments could be given depending on the severity, cause, and type of stroke (1).
- Oxygen supplementation
- Antiepileptic (anti-seizure) medications for teens who have seizures
- Medications to eliminate blood clots
- Blood thinners
- Blood transfusions
- Surgery for brain injuries or to correct heart defects
- Repair of affected blood vessels
Most teens recover from a stroke without complications if they receive necessary and timely medical care. Teens may require special care for movement, learning, behavioral issues, speech, and vision after the initial stabilization treatment. Speech therapists, psychiatrists, physical therapists, and occupational therapists can train your teen to overcome these issues.
Prevention Of Stroke In Teens
Image: IStock
Stroke may not be preventable in all cases. However, children with known risk factors could follow necessary precautions to avoid stroke. Appropriate treatment of clotting disorders and sickle cell anemia may reduce the risk of these conditions.
Cardiovascular check-ups and regular medications for teens with heart problems may help prevent cardiac reasons for stroke. Teens who have a history of stroke must take the prescribed medications to avoid a second stroke.
Frequently Asked Questions
1. What are the signs of a silent stroke?
A silent stroke occurs in a deeper region of the brain called basal ganglia. It does not manifest typical stroke symptoms such as poor vision, paralysis, or speech impairment. Hence, there are no noticeable signs of a silent stroke (6).
2. Can stress cause a stroke?
Yes, stress may trigger or increase the risk of stroke by causing blood clots and poor blood flow to the heart (7).
3. What are the long-term effects of strokes in teenagers?
Long-term effects of stroke in teenagers may vary depending on the stroke severity, the area of the brain affected, and the individual’s overall health. Still, some potential long-term effects of stroke might include problems with personality, intellectual abilities, and emotional regulation. Other possible effects include short-term memory loss, problems with language, and difficulty in swallowing (10).
4. What are the psychological impacts of strokes in teenagers?
A stroke is a sudden and unexpected event that can significantly affect a teen’s mental health. After a stroke, a teen may experience a range of emotions, such as confusion, forgetfulness, irritability, depression, and anxiety. These emotional changes can also affect physical and social issues, resulting in adjustment difficulties (11).
5. What are the differences between strokes in teenagers and adults?
The risk factors associated with strokes in adults are significantly different from those of teenagers. The common risk factors for strokes in adults include high blood pressure, diabetes, age, and excessive smoking (12).
6. What is the rate of strokes in teenagers compared to adults?
Although the occurrence of strokes in teenagers is fairly uncommon, they usually comprise about 10-15% of all stroke cases (13).
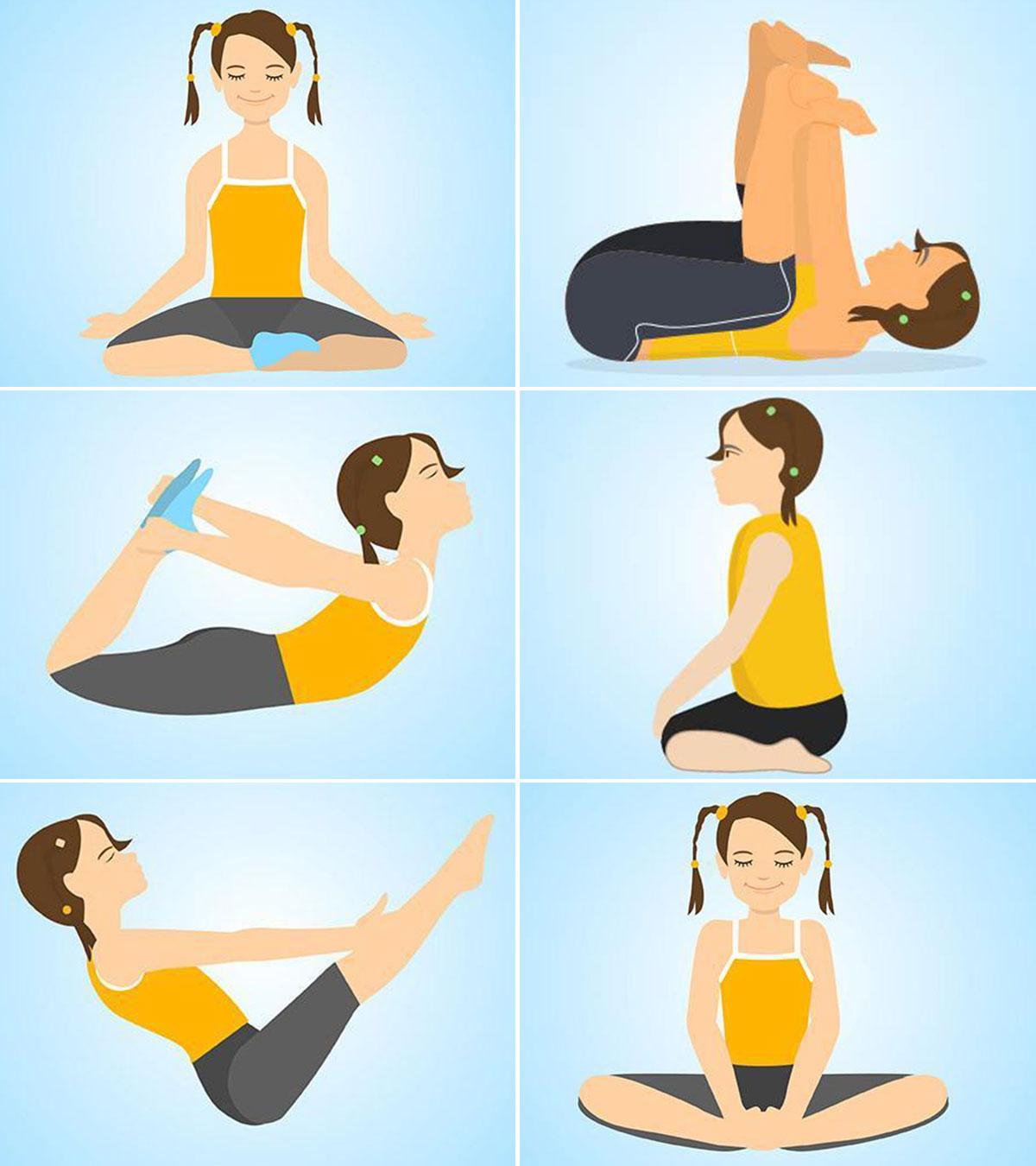
7. Are there any lifestyle changes to reduce the risk of strokes in teenagers?
Maintaining a healthy weight, eating a well-balanced diet low in saturated fats, trans fat, and cholesterol, engaging in regular physical activities, and avoiding smoke and alcohol are some pertinent lifestyle changes that can help reduce stroke risk in adolescents (14).
8. What emotional and psychological support is available for teenagers who have had strokes?
Family and friends are the main source of psychological and emotional support for teens who had strokes. Individual counseling or therapy sessions with a mental health professional is another way a teen can share their thoughts and experiences. They can also join a support group where they can share experiences and receive emotional support. Stroke rehabilitation programs and numerous online resources, websites, and forums also offer support and information for teenagers who have had strokes (15).
Stroke is a heart disease that can affect anyone. But people with risk factors such as head injury, blood or genetic disorder, congenital disabilities, or blood vessel abnormalities may be more vulnerable. Since stroke in teenagers is mostly not preventable, it is important to be aware of its signs to seek immediate medical help. Timely intervention can prevent unfortunate outcomes, and brain retraining in the recovery period can help teens get back to their normal body functioning. Remember, they require your utmost support and care for easier and smooth healing during this period.
Infographic : What Are The Benefits Of Long-term Therapies For Stroke In Children?
Long-term rehabilitation therapies are needed to obtain complete functional recovery after a stroke. These therapies retrain the brain and vary depending on the brain’s affected area. The duration of therapies can be different in each case. Go through the infographic to know the benefits of long-term therapies for your child after recovering from a stroke. Illustration: Momjunction Design Team
Key Pointers
- A stroke can occur if there is a blockage or delay in the blood supply to the brain.
- Depending on the blood vessel location, your teen may have an ischemic or hemorrhagic stroke.
- Remember the acronym FAST for face drooping, arm weakness, speech difficulty, and time to call 911.
- Mini-strokes usually are harmless, but severe strokes for extended periods may result in irreversible brain damage.
Image: Stable Diffusion/MomJunction Design Team
Strokes in teens may be caused by a number of reasons. Learn how to recognize the signs and get timely help with this video.
References
1. Pediatric Stroke; Johns Hopkins Medicine
2. Pediatric Stroke Type, Causes, & Symptoms; Children’s Hospital Pittsburgh
3. Pediatric and Adolescent Stroke; Memorial Hermann
4. Stroke In Children; Lucile Packard Children’s Hospital Stanford
5. Complications After Stroke; American Heart Association
6. Silent strokes; Boston University
7. Stress Can Increase Your Risk for Heart Disease; University of Rochester Medical center
8. Pediatric & Adolescent Stroke; Memorial Hermann
9. Stroke; Raising Children10. Long-term Effects of Stroke; Christiana Care11. Emotional & Behavioral Effects of Stroke; American Stroke Association.12. Guidelines Highlight Key Differences Between Child and Adult Stroke; Nationwide Children’s13. Dževdet Smajlović; 2015; Strokes in young adults: epidemiology and prevention; Pubmed14. Prevent Stroke: What You Can Do; CDCising Childre15. Mental Health Following A Stroke; UT Health Houston
Read full bio of Maria Carmela Villania-Mamauag
Read full bio of Dr. Ritika Shah
Read full bio of Shinta Liz Sunny